The 5 Nursing Process Steps – (Learn Each Step in Detail)

One of the most important tools a nurse can use in practice is the nursing process. Although nursing schools teach first-year students about the nursing process, some nurses fail to grasp the impact its proper use can have on patient care. In this article, I will share information about the nursing process, its history, its purpose, its main characteristics, and the 5 steps involved in carrying out the nursing process. After reading this article, you will be able to answer the question, “what is the nursing process” and understand what is involved in each of the 5 steps of the nursing process. Additionally, throughout this article, after discussing a step of the nursing process, I will share an example of how the nurse would proceed with that step. For this article’s purposes, we will use information about the following patient: Mr. Collie, a fifty-four-year-old white male being admitted to the Medical-Surgical floor for acute congestive heart failure.

What is the Nursing Process in Simple Words?
When was the nursing process developed, who developed the nursing process, what is the purpose of the nursing process, what are the 7 main characteristics of the nursing process, 1. within the legal scope of practice, 2. based on sound knowledge, 4. client-centered, 5. goal-directed, 6. prioritized, 7. dynamic and cyclical, how many steps are there in the nursing process, what are the 5 steps of the nursing process, step #1: assessment phase, step #2: diagnosis phase, step #3: planning phase, step #4: implementation phase, step #5: evaluation phase, useful resources to gain more information about the nursing process, blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. how is nursing process different from the scientific method, 2. do all nurses use the nursing process, 3. do doctors also use the nursing process, 4. what does adpie stand for, 5. is it always necessary for a nurse to follow all steps of the nursing process, 6. how does critical thinking impact the nursing process, 7. how does a health information system affect the nursing process, 8. how to use maslow hierarchy in the nursing process, 9. which nursing process step includes tasks that can be delegated, 10. which nursing process step includes tasks that cannot be delegated, 11. how does the nursing process apply to pharmacology.

The Nursing Process: A Comprehensive Guide
In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse ‘s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
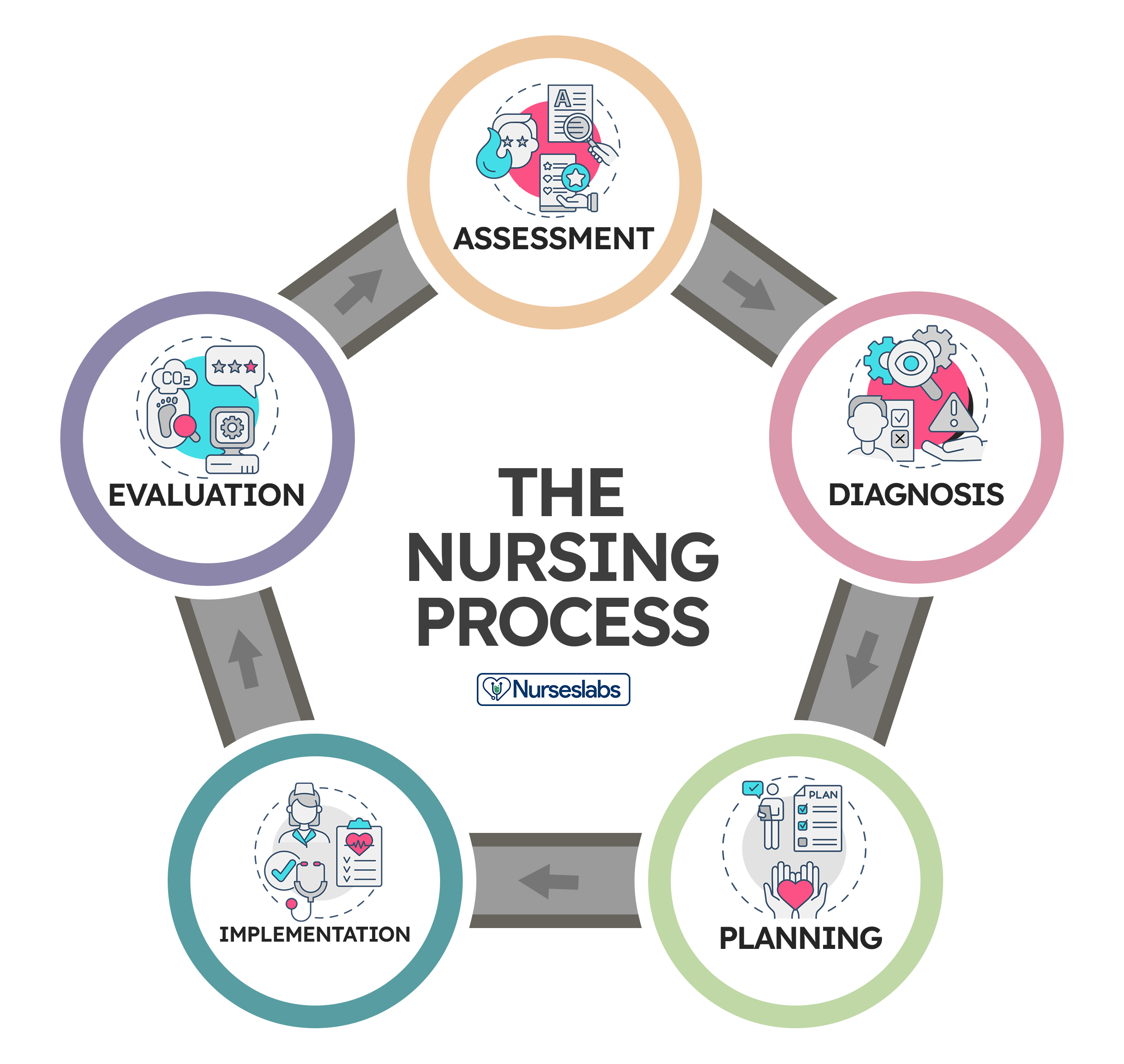
Application of the fundamental principles of critical thinking , client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data.
- 2. Diagnosis: “What is the problem?”
Initial Planning
Ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care .
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation . The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch , smell , or hearing , and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature , pulse, and respiratory rates, blood pressure , vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance , facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members , support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history , which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation .
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste ) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature .
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
2. Diagnosis: “What is the problem?”
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care .
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions . When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement , and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation: “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration, educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking , to reduce the patient’s anxiety , anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing , administering an injection, manipulating equipment, bandaging, moving , lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non- RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory, nursing practice , and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation: “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan , and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan .
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.

41 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Very helpful Thank you
This is a wonderful and very useful article! I was wondering if the image under the “What is the Nursing Process?” is copyright protected? If yes, by who? Thank you!!
Feel free to use :)
Leave a Comment Cancel reply

Assignment/Delegation
Assignment and delegation are essential components of leadership and management in nursing, ensuring safe and efficient patient care delivery. For the NCLEX-RN®, understanding these concepts helps nurses prioritize tasks, utilize team members effectively, and maintain accountability. Assignment involves distributing tasks based on scope of practice, while delegation requires transferring responsibilities while ensuring proper oversight. Mastering these skills enables nurses to make informed decisions, promote teamwork, and enhance patient outcomes, all of which are critical for success in the NCLEX-RN® exam.
Learning Objectives
In studying “Leadership & Management: Assignment/Delegation” for the NCLEX-RN® exam, you should learn to understand the principles of assigning and delegating tasks among healthcare team members. Analyze the Five Rights of Delegation and how they ensure safe, effective patient care. Evaluate the roles and scope of practice for RNs, LPNs, and UAPs to prioritize and allocate care activities appropriately. Explore frameworks like Maslow’s Hierarchy of Needs and the ABCs to guide decision-making. Apply these concepts to clinical scenarios, ensuring accountability, effective communication, and supervision, and interpret questions that test these principles in practice passages to enhance exam readiness.
Key Concepts of Assignment and Delegation
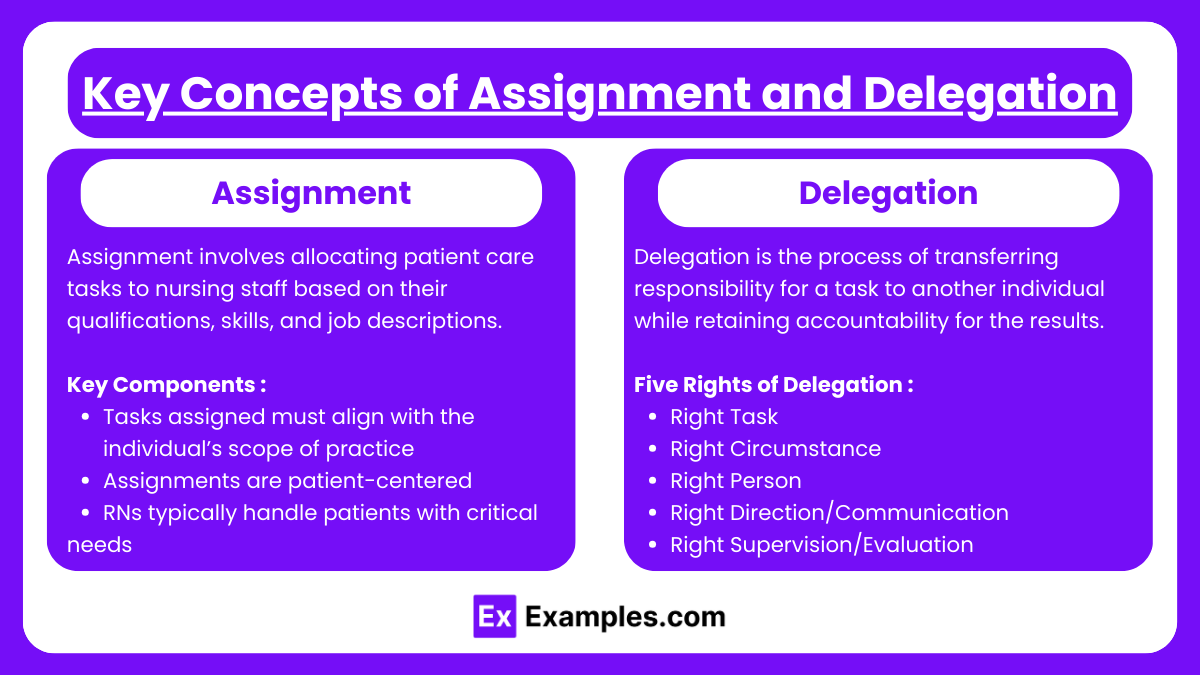
1. Assignment
- Assignment involves allocating patient care tasks to nursing staff based on their qualifications, skills, and job descriptions.
- Tasks assigned must align with the individual’s scope of practice and legal parameters as outlined in the Nurse Practice Act.
- Assignments are patient-centered, focusing on the needs of the individual while optimizing the efficiency of the care team.
- RNs typically handle patients with critical or complex needs, while LPNs and UAPs manage stable patients requiring predictable care.
2. Delegation
- Delegation is the process of transferring responsibility for a task to another individual while retaining accountability for the results.
- Right Task : Only delegate tasks that can safely be performed by another individual within their scope of practice.
- Right Circumstance : Delegate only when the patient’s condition is stable and predictable.
- Right Person : Choose a delegatee who possesses the necessary skills and training.
- Right Direction/Communication : Provide clear, detailed instructions, including the expected outcomes and any necessary follow-up.
- Right Supervision/Evaluation : Monitor the task’s completion and evaluate outcomes to ensure quality care.
- Delegation Challenges : Miscommunication, lack of training, or unclear expectations can compromise patient safety. Effective leadership is essential to prevent such issues.
Principles in Assignment
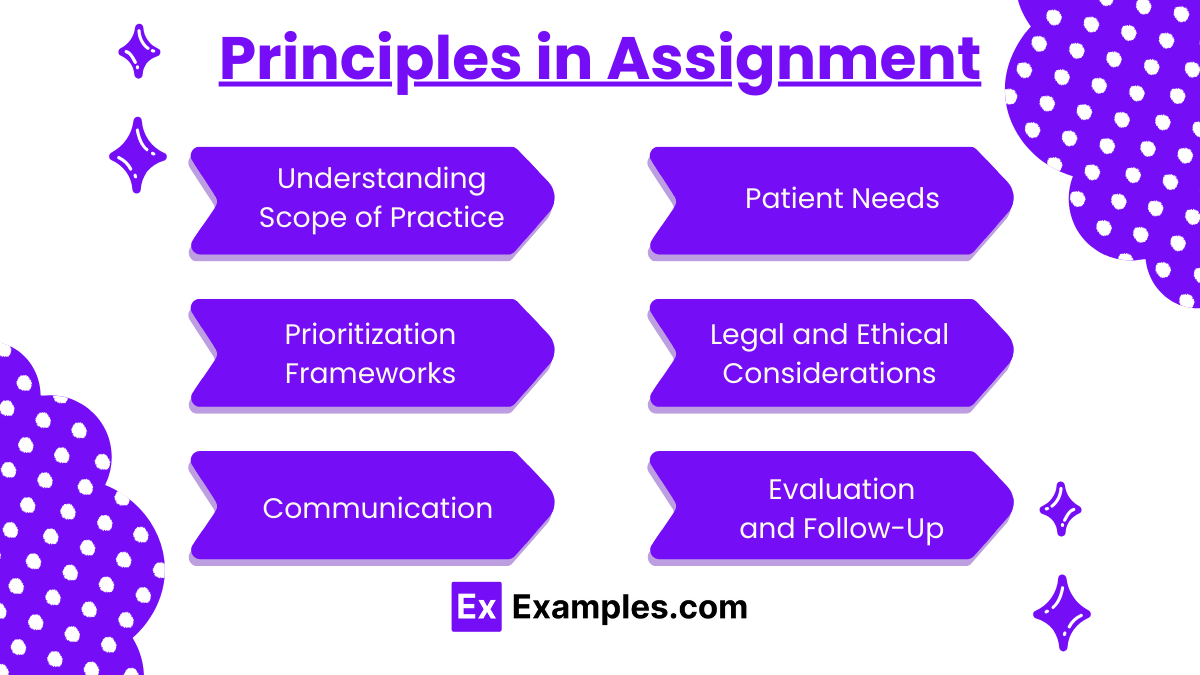
1. Understanding Scope of Practice
- Assign tasks based on the legal and professional scope of the team members.
- Ensure tasks align with the Nurse Practice Act and job descriptions.
- Recognize that RNs manage patients with complex needs, while LPNs/LVNs handle routine care, and UAPs assist with non-clinical tasks.
2. Patient Needs
- Match the complexity of patient care with the skill and competence of the assigned staff.
- Critical or unstable patients should remain under the care of an RN.
- Stable patients with predictable outcomes can be assigned to LPNs or UAPs.
3. Prioritization Frameworks
- Use Maslow’s Hierarchy of Needs, ABCs (Airway, Breathing, Circulation), and Safety to assign tasks that ensure immediate life-threatening conditions are addressed first.
- Ensure all assignments reflect patient safety and continuity of care.
4. Legal and Ethical Considerations
- Assignments must comply with institutional policies and state regulations.
- Avoid overloading staff, as this can compromise patient safety and quality of care.
- Ensure that assignments are equitable and promote teamwork.
5. Communication
- Provide clear, concise, and detailed instructions regarding the expectations of the assigned tasks.
- Include necessary patient-specific information, such as care plans, goals, and timelines.
6. Evaluation and Follow-Up
- Continuously monitor and evaluate the outcomes of the assigned tasks.
- Provide constructive feedback to the team and address any issues that arise.
- Ensure tasks are completed as per standards, and make adjustments to assignments if necessary to maintain patient safety and care quality.
Principles in Delegation

1. The Five Rights of Delegation
- Right Task : Ensure the task is appropriate for delegation based on patient condition and staff competence.
- Right Circumstance : Only delegate when the patient’s condition is stable and the task does not require clinical judgment.
- Right Person : Delegate to individuals who have the necessary training, knowledge, and skills.
- Right Direction/Communication : Provide clear, specific instructions and expectations, ensuring the delegatee fully understands.
- Right Supervision/Evaluation : Monitor the delegatee’s progress, provide feedback, and assess outcomes.
2. Accountability and Responsibility
- The RN retains accountability for the overall care plan and the outcomes of the delegated task.
- Delegate tasks only to individuals who are competent and confident in performing them.
- Ensure continuous supervision and support, intervening as necessary.
3. Building Trust and Teamwork
- Delegation requires a relationship of mutual trust between the RN and team members.
- Promote an environment where staff feel comfortable seeking clarification or reporting challenges.
- Use delegation as an opportunity to develop team members’ skills and confidence.
4. Recognizing Limitations
- Avoid delegating tasks requiring critical thinking, clinical judgment, or nursing assessments.
- Do not delegate activities that require specialized knowledge, such as patient education or managing a deteriorating patient.
5. Effective Supervision
- Regularly check on progress and provide guidance as needed.
- Evaluate outcomes and use them as a basis for improving future delegation practices.
- Offer feedback and acknowledgment to foster staff motivation and growth.
Example 1: Prioritizing Care in a Multi-Patient Assignment
An RN is managing a medical-surgical unit with a mix of stable and unstable patients. The RN assigns the care of two stable postoperative patients to the LPN. These patients require routine medication administration and basic wound care. The RN retains responsibility for a critically ill patient who requires frequent monitoring, titration of IV medications, and assessments. This prioritization ensures that complex tasks requiring clinical judgment are handled by the RN, while routine care is safely assigned to the LPN.
Example 2: Delegating Non-Clinical Tasks to UAPs
During a busy shift, the RN delegates non-clinical tasks such as assisting patients with bathing, feeding, and ambulation to the UAP. The RN provides clear instructions, such as reporting any changes in the patient’s condition (e.g., difficulty breathing during ambulation). This delegation allows the RN to focus on higher-priority clinical tasks, such as administering medications and assessing unstable patients.
Example 3: Managing a Patient Discharge
The RN is preparing a patient for discharge. The RN retains responsibility for providing discharge teaching, including medication instructions and follow-up care, as this task requires clinical judgment and patient education. The RN delegates the task of gathering the patient’s belongings and escorting them to their transportation to the UAP. This ensures efficient workflow while maintaining high-quality patient care.
Example 4: Handling a Code Situation
During a cardiac arrest in the unit, the RN takes charge of the situation, directing the resuscitation efforts and administering critical medications. The RN delegates tasks such as compressions to a trained UAP and asks an LPN to monitor and document the patient’s vital signs and response during the event. Effective communication and supervision ensure that each team member performs their role appropriately, contributing to the patient’s survival.
Example 5: Delegating Routine Procedures
The RN assigns the task of inserting a urinary catheter for a stable patient to the LPN, as this task falls within the LPN’s scope of practice. The RN ensures the LPN understands the procedure and the expected outcomes. After the task is completed, the RN evaluates the patient’s response to the intervention, maintaining accountability for the overall care.
Practice Questions
A registered nurse (RN) is delegating tasks to a licensed practical nurse (LPN) and unlicensed assistive personnel (UAP). Which task should the RN delegate to the UAP?
A. Administering oral medications to a stable patient B. Performing a sterile dressing change on a post-operative patient C. Assisting a patient with ambulation to the bathroom D. Conducting a focused assessment on a patient with chest pain
Answer: C. Assisting a patient with ambulation to the bathroom
Explanation:
- UAP Scope of Practice : UAPs are trained to perform non-clinical, routine tasks that do not require clinical judgment, such as ambulating, bathing, and feeding patients.
- LPN Responsibilities : Administering oral medications (A) and performing sterile dressing changes (B) fall within the scope of LPN practice.
- RN Responsibilities : Conducting focused assessments (D) involves clinical judgment, which is the responsibility of the RN.
- Delegating ambulation to the UAP allows the RN to focus on tasks requiring higher-level decision-making.
The RN on a medical-surgical unit is assigning patients to the care team. Which patient should the RN assign to the LPN?
A. A patient admitted with unstable angina who is scheduled for a stress test B. A patient receiving IV chemotherapy with a history of allergic reactions C. A patient requiring frequent blood glucose monitoring and insulin administration D. A patient newly diagnosed with a pulmonary embolism receiving IV heparin
Answer: C. A patient requiring frequent blood glucose monitoring and insulin administration
- Stable Patient : LPNs can care for stable patients with predictable outcomes, such as monitoring blood glucose and administering subcutaneous insulin.
- Critical and Complex Care : Patients with unstable angina (A), potential chemotherapy reactions (B), or a new pulmonary embolism on IV heparin (D) require ongoing assessment and critical thinking, which are within the RN’s scope.
- Assigning stable patients to the LPN ensures safe delegation and prioritizes the RN’s role in handling higher-acuity cases.
Which of the following statements indicates the RN understands the “Right Supervision/Evaluation” principle of delegation?
A. “I will provide detailed instructions to the LPN and let them complete the task independently.” B. “I will verify that the task was completed correctly and provide feedback as necessary.” C. “I will assume the LPN knows how to handle the task because they are experienced.” D. “I will only follow up with the LPN if the patient complains about the task.”
Answer: B. “I will verify that the task was completed correctly and provide feedback as necessary.”
- Right Supervision/Evaluation : Delegation requires the RN to monitor the task’s completion, ensure it was performed correctly, and provide guidance or feedback as needed.
- Option A : While detailed instructions are important, supervision and follow-up are still necessary.
- Option C : Assumptions about the delegatee’s experience without verification can compromise patient safety.
- Option D : Waiting for a patient complaint to evaluate task performance neglects the RN’s responsibility for oversight.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Nursing process.
Tammy J. Toney-Butler ; Jennifer M. Thayer .
Affiliations
Last Update: April 10, 2023 .
- Introduction
In 1958, Ida Jean Orlando started the nursing process that still guides nursing care today. Defined as a systematic approach to care using the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EDP) recommendations, and nursing intuition. Holistic and scientific postulates are integrated to provide the basis for compassionate, quality-based care. [1] [2] [3]
The nursing process functions as a systematic guide to client-centered care with 5 sequential steps. These are assessment, diagnosis, planning, implementation, and evaluation.
Assessment is the first step and involves critical thinking skills and data collection; subjective and objective. Subjective data involves verbal statements from the patient or caregiver. Objective data is measurable, tangible data such as vital signs, intake and output, and height and weight.
Data may come from the patient directly or from primary caregivers who may or may not be direct relation family members. Friends can play a role in data collection. Electronic health records may populate data and assist in assessment.
Critical thinking skills are essential to assessment, thus the need for concept-based curriculum changes.
The formulation of a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The North American Nursing Diagnosis Association (NANDA) provides nurses with an up-to-date list of nursing diagnoses. A nursing diagnosis, according to NANDA, is defined as a clinical judgment about responses to actual or potential health problems on the part of the patient, family, or community.
A nursing diagnosis encompasses Maslow's Hierarchy of Needs and helps to prioritize and plan care based on patient-centered outcomes. In 1943, Abraham Maslow developed a hierarchy based on basic fundamental needs innate to all individuals. Basic physiological needs/goals must be met before higher needs/goals can be achieved such as self-esteem and self-actualization. Physiological and safety needs provide the basis for the implementation of nursing care and nursing interventions. Thus, they are at the base of Maslow's pyramid, laying the foundation for physical and emotional health. [4] [5]
Maslow's Hierarchy of Needs
- Basic Physiological Needs: Nutrition (water and food), elimination (Toileting), airway (suction)-breathing (oxygen)-circulation (pulse, cardiac monitor, blood pressure) (ABCs), sleep, sex, shelter, and exercise.
- Safety and Security: Injury prevention (side rails, call lights, hand hygiene, isolation, suicide precautions, fall precautions, car seats, helmets, seat belts), fostering a climate of trust and safety (therapeutic relationship), patient education (modifiable risk factors for stroke, heart disease).
- Love and Belonging: Foster supportive relationships, methods to avoid social isolation (bullying), employ active listening techniques, therapeutic communication, and sexual intimacy.
- Self-Esteem: Acceptance in the community, workforce, personal achievement, sense of control or empowerment, accepting one's physical appearance or body habitus.
- Self-Actualization: Empowering environment, spiritual growth, ability to recognize the point of view of others, reaching one's maximum potential.
The planning stage is where goals and outcomes are formulated that directly impact patient care based on EDP guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual's unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Goals should be:
- Measurable or Meaningful
- Attainable or Action-Oriented
- Realistic or Results-Oriented
- Timely or Time-Oriented
Implementation
Implementation is the step that involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This phase requires nursing interventions such as applying a cardiac monitor or oxygen, direct or indirect care, medication administration, standard treatment protocols, and EDP standards.
This final step of the nursing process is vital to a positive patient outcome. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. Reassessment may frequently be needed depending upon overall patient condition. The plan of care may be adapted based on new assessment data.
- Issues of Concern
According to a 2011 study conducted in Mekelle Zone hospitals, nurses lack the knowledge to implement the nursing process into practice and factors such as nurse-patient ratios inhibit them from doing so. Ninety percent of study participants lacked sufficient experience to apply the nursing process to standard practice. The study also concluded that a shortage of available resources, coupled with increased workloads due to high patient-nurse ratios, contributed to the lack of the nursing process implementation in the delivery of patient care. [6] [7] [8]
- Clinical Significance
The utilization of the nursing process to guide care is clinically significant going forward in this dynamic, complex world of patient care. Aging populations carry with them a multitude of health problems and inherent risks of missed opportunities to spot a life-altering condition.
As explored by Salmond and Echevarria, healthcare is changing, and the traditional roles of nurses are transforming to meet the demands of this new healthcare environment. Nurses are in a position to promote change and impact patient delivery care models in the future. [9] [10]
- Other Issues
Critical thinking skills will play a vital role as we develop plans of care for these patient populations with multiple comorbidities and embrace this challenging healthcare arena. Thus, the trend towards concept-based curriculum changes will assist us in the navigation of these uncharted waters.
Concept-Based Curriculum
Baron further explores this need for a concept-based curriculum as opposed to the traditional educational model and the challenges faced with its implementation. A direct impact on quality patient care and positive outcomes. Nursing practice and educational environments form a bond with clinical knowledge and expertise, and that bond facilitates the transition into the current workforce as an indispensable team player and leader in this new wave of healthcare.
Learning should be the focus and the integration into current practice. Learning is a dynamic process, propelled by a force that must coexist within the same learning milieu between educator and student, preceptor and novice, mentor, and trainee.
IN the future, nurses must be able to problem-solve in a multitude of situations and conditions to meet these new adversities: challenging nurse-patient ratios, multifaceted approaches to prioritization of care, fewer resources, navigation of the electronic health record as well as functionality within the team dynamic and leadership style.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Maslow's Hierarchy of Needs for Nursing Contributed by Tammy J. Toney-Butler, AS, RN, CEN, TCRN, CPEN
Disclosure: Tammy Toney-Butler declares no relevant financial relationships with ineligible companies.
Disclosure: Jennifer Thayer declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Toney-Butler TJ, Thayer JM. Nursing Process. [Updated 2023 Apr 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Contributions of Jean Watson's theory to holistic critical thinking of nurses. [Rev Bras Enferm. 2018] Contributions of Jean Watson's theory to holistic critical thinking of nurses. Riegel F, Crossetti MDGO, Siqueira DS. Rev Bras Enferm. 2018 Jul-Aug; 71(4):2072-2076.
- Review Evidence for practice, epistemology, and critical reflection. [Nurs Philos. 2006] Review Evidence for practice, epistemology, and critical reflection. Avis M, Freshwater D. Nurs Philos. 2006 Oct; 7(4):216-24.
- Use of the Watson-Glaser Critical Thinking Appraisal with BSN students. [Nurs Health Care Perspect. 1999] Use of the Watson-Glaser Critical Thinking Appraisal with BSN students. Frye B, Alfred N, Campbell M. Nurs Health Care Perspect. 1999 Sep-Oct; 20(5):253-5.
- Review Statement on nursing: a personal perspective. [Gastroenterol Nurs. 2004] Review Statement on nursing: a personal perspective. McCutcheon T. Gastroenterol Nurs. 2004 Sep-Oct; 27(5):226-9.
- Review Holistic assessment and care: presence in the process. [Nurs Clin North Am. 2007] Review Holistic assessment and care: presence in the process. Potter PJ, Frisch N. Nurs Clin North Am. 2007 Jun; 42(2):213-28, vi.
Recent Activity
- Nursing Process - StatPearls Nursing Process - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients' well-being and health. This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care. ... The assignment of the performance of activities or ...
The nursing process is a dynamic process as it is constantly affected by the patient's needs, circumstances impacting their needs, and the environment in which care is applied. It encompasses emotional, physical, social, and medical aspects. ... Delegation involves the assignment of specific tasks or activities related to patient care to ...
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse's critical thinking to provide the best care possible to the client.. What is the purpose of the nursing process? The following are the purposes of the nursing ...
Allen SB. Assignments matter: Results of a nurse-patient assignment survey. MEDSURG Nurs[in press]. American Nurses Association (ANA). ANA's Principles for Nurse Staffing. 2nd ed. Silver Spring, MD: ANA; 2012. Your nurse-patient assignment process may be dictated by unit layout, patient census, or nurse-to-patient ratio.
Study with Quizlet and memorize flashcards containing terms like A client comes to the walk-in clinic with reports of abdominal pain and diarrhea. While taking the client's vital signs, the nurse is implementing which phase of the nursing process? A. Assessment B. Diagnosis C. Planning D. Implementation, The nurse is measuring the client's urine output and straining the urine to assess for stones.
Assignment and delegation are essential components of leadership and management in nursing, ensuring safe and efficient patient care delivery. For the NCLEX-RN®, understanding these concepts helps nurses prioritize tasks, utilize team members effectively, and maintain accountability. ... Delegation is the process of transferring responsibility ...
The common thread uniting different types of nurses who work in varied areas is the nursing process—the essential core of practice for the registered nurse to deliver holistic, patient-focused care. Assessment An RN uses a systematic, dynamic way to collect and analyze data about a client, the first step in delivering nursing care.
In 1958, Ida Jean Orlando started the nursing process that still guides nursing care today. Defined as a systematic approach to care using the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EDP) recommendations, and nursing intuition. Holistic and scientific postulates are integrated to provide the basis for ...
The assignment process requires constant evaluation and reevaluation of information and priorities. And that's why the assignments are usually written in pencil on paper or in marker on a dry-erase board. As the charge nurse, you must communicate with patients and staff throughout the shift and react to changing needs by updating assignments.
tive on the nurse's role and the assignment process. Instructions for Continuing Nursing Education Contact Hours appear on page 82. 78 March-April 2018 • Vol. 27/No. 2