An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

The abortion and mental health controversy: A comprehensive literature review of common ground agreements, disagreements, actionable recommendations, and research opportunities
David c reardon.
- Author information
- Article notes
- Copyright and License information
David C Reardon, Elliot Institute, PO Box 7348, Springfield, IL 62791, USA. Email: [email protected]
Received 2018 Jun 19; Accepted 2018 Sep 26; Collection date 2018.
This article is distributed under the terms of the Creative Commons Attribution 4.0 License ( http://www.creativecommons.org/licenses/by/4.0/ ) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages ( https://us.sagepub.com/en-us/nam/open-access-at-sage ).
The abortion and mental health controversy is driven by two different perspectives regarding how best to interpret accepted facts. When interpreting the data, abortion and mental health proponents are inclined to emphasize risks associated with abortion, whereas abortion and mental health minimalists emphasize pre-existing risk factors as the primary explanation for the correlations with more negative outcomes. Still, both sides agree that (a) abortion is consistently associated with elevated rates of mental illness compared to women without a history of abortion; (b) the abortion experience directly contributes to mental health problems for at least some women; (c) there are risk factors, such as pre-existing mental illness, that identify women at greatest risk of mental health problems after an abortion; and (d) it is impossible to conduct research in this field in a manner that can definitively identify the extent to which any mental illnesses following abortion can be reliably attributed to abortion in and of itself. The areas of disagreement, which are more nuanced, are addressed at length. Obstacles in the way of research and further consensus include (a) multiple pathways for abortion and mental health risks, (b) concurrent positive and negative reactions, (c) indeterminate time frames and degrees of reactions, (d) poorly defined terms, (e) multiple factors of causation, and (f) inherent preconceptions based on ideology and disproportionate exposure to different types of women. Recommendations for collaboration include (a) mixed research teams, (b) co-design of national longitudinal prospective studies accessible to any researcher, (c) better adherence to data sharing and re-analysis standards, and (d) attention to a broader list of research questions.
Keywords: Abortion mental health, abortion, reproductive health, post-abortion trauma, research bias, complicated grief, ambiguous loss, bereavement, post-traumatic stress disorder, pregnancy loss
Introduction
In 1992, the Journal of Social Issues dedicated an entire issue to the psychological effects of induced abortion. In an overview of the contributors’ papers, the editor, Dr Gregory Wilmoth, concluded,
There is now virtually no disagreement among researchers that some women experience negative psychological reactions postabortion. Instead the disagreement concerns the following: (1) The prevalence of women who have these experiences …, (2) The severity of these negative reactions …, (3) The definition of what severity of negative reactions constitutes a public health or mental health problem …, [and] (4) The classification of severe reactions … 1
Twenty-six years later, the body of literature has grown. Today, there are many additional areas of agreement, but the areas of disagreement have also grown.
As with most controversies, the abortion and mental health (AMH) controversy is driven by at least two different perspectives regarding how best to interpret accepted facts. A useful parallel is found in the debate over climate change. On the fringes of the climate change controversy are non-experts who hold an extreme position of either total denial or total credulity. But it is far more common for skeptics to acknowledge that fossil fuels make some contribution to global warming while still arguing that these effects are not as extreme global warming proponents contend. 2 This group may be described as global warming minimalists. Their normal pattern is to interpret the data in a way that minimizes the potential threat. By contrast, global warming proponents may be more likely to interpret the data in ways that emphasize the potential risks.
Similarly, in regard to the AMH controversy, there are both AMH minimalists and AMH proponents. The experts from both groups can report similar findings from the same data but will do so in ways that seem to either minimize or emphasize the negative outcomes associated with abortion. It should be carefully noted that there is actually a broad spectrum of expert views regarding the AMH link. 3 While each researcher and expert has likely developed carefully considered and nuanced opinions, these have not been completely disclosed and cannot be cataloged in regard to every issue discussed herein. Still, broadly speaking, it is evident that both expert reviews and the authors of individual studies appear to generally support either the view that (a) the mental health effects associated with abortion are minimal and within the expected range for the women seeking abortions 4 – 10 or (b) the effects are significant enough to justify more research dollars, and better screening and counseling in order to reduce the number of adverse outcomes. 11 – 19 In addressing this conflict, it is not my intention to pigeonhole any particular expert’s viewpoint at any location on the spectrum of views regarding AMH.
In writing this review, I have tried to be as objective and fair as possible. Yet, as discussed later, since my own informed opinion is also influenced by my own experiences and preconceptions, full disclosure requires that I acknowledge at the outset that I fit most closely under the category of an AMH proponent. That said, my goal is not to dismiss or disprove the viewpoint of “the other side,” but rather to understand and engage with it in a manner that will contribute to a respectful “transformational dialogue” that will help to “crystalize the areas of agreement and disagreement along with opportunities for collaboration.” 20 In this regard, it is my great hope that those who disagree with my analysis and conclusions herein will use the publication of this review as an opportunity to publish responses and reviews that address the issues raised with additional depth from their perspectives.
The method I used for this review was to carefully examine previous literature reviews regarding mental health effects associated with legal abortion that have been published since 2005. 4 – 10 , 12 – 19 , 21 , 22 In that sense, this article may be considered a review of reviews of the literature on AMH. In addition, I studied the references cited in these various reviews in order to further my effort to more completely identify (a) areas of agreement and disagreement, (b) the underlying reasons for disagreements, and (c) opportunities to collaborate in light of the current literature.
This undertaking is intended to advance more than just an academic discussion, however. Research has shown that women considering abortion have a high degree of desire for information on “all possible complications,” including rare risks. 23 Therefore, an updated and more complete understanding of the literature can and should better prepare physicians and mental healthcare providers with more accurate and helpful information for advising and counseling women before or after an abortion. For example, better screening for risk factors should help to identify women who may benefit from additional pre- or post-abortion counseling 24 – 38 and may also help to prevent cases of women being pressured into unwanted abortions. In addition, more complete insights may help mental health counselors to be more aware and sensitive to providing the counseling services that women want and need.
This review is organized into three sections. The first examines major areas of agreement and offers a synthesis of the findings from major studies. The second section investigates the obstacles to building a consensus between AMH minimalists and AMH proponents, including institutional and ideological biases, research obstacles, poorly defined terms, and similar issues that contribute to the disparity in the conclusions most emphasized by each side. The third section provides recommendations for collaborative research based on the insights gained from the first two sections, addressing such issues as data sharing, mixed research teams, and how to maximize the value of longitudinal prospective studies.
Areas of agreement
Abortion contributes to negative outcomes for at least some women.
The 2008 report of the American Psychological Association’s (APA) Task Force on Mental Health and Abortion (TFMHA) concluded that “it is clear that some women do experience sadness, grief, and feelings of loss following termination of a pregnancy, and some experience clinically significant disorders, including depression and anxiety.” 4 Indeed, task force chair Brenda Major et al.’s 39 own research had reported that 2 years after their abortions, 1.5% of the remnant participating in her case series (38% of the 1177 eligible women, after dropouts) had all the symptoms for abortion-specific post-traumatic stress disorder (PTSD). In addition, she found that compared to their 1-month post-abortion assessments, at 2 years the participating remnant had significantly rising rates of depression and negative reactions and lowering rates of positive reactions, relief, and decision satisfaction. 39
The fact that some women do have maladjustments is most specifically documented in case studies developed by post-abortion counselors successfully treating women with maladjustments, including counselors working from a pro-choice perspective 40 – 44 as well as from those working from a pro-life perspective. 45 – 47
Even one of the harshest critics of the “myth” of abortion trauma, psychiatrist Nada L Stotland, 40 subsequently reported her own clinical experience treating a patient whose miscarriage triggered a mental health crisis arising from unresolved issues regarding a prior abortion. Stotland, who later served as president of the American Psychiatric Association, subsequently began to recommend screening of prospective abortion patients for risk factors in order to guide decision counseling and identify additional counseling needs. 31
Some groups of women are predictably at greater risk of negative outcomes
There is a strong research-based consensus that there are numerous risk factors that can be used to identify which women are at greatest risk of negative psychological outcomes following one or more abortions. Indeed, the TFMHA concluded that one of the few areas of research which can be most effectively studied is in regard to efforts to “identify those women who might be more or less likely than others to show adverse or positive psychological outcomes following an abortion.” 4
The TFMHA itself identified at least 15 risk factors for increased risk of negative reactions. While the TFMHA did not report on the percentage of women exhibiting each risk factor, Table 1 provides ranges of the incidence of each TFMHA risk factor as reported in the literature. The incidence rates shown in Table 1 clearly suggest that the majority of women seeking abortion have one or more of the TFMHA identified risk factors. Since exposure to multiple abortions is one of the risk factors, that risk factor alone applies to approximately half of all women having abortions, at least in the United States. 64
Risk factors for mental health problems after an abortion identified by the American Psychological Association’s Task Force on Mental Health and Abortion (TFMHA) in 2008.
Notably, the TFMHA list used here is one of the shortest that has been developed. A similar, but longer list is published in the text book on abortion most highly recommended by the National Abortion Federation. 66 A more recent systematic search of the literature for risk factors associated with elevated rates of psychological problems after abortion cataloged 119 peer reviewed studies identifying 146 individual risk factors which the author grouped into 12 clusters. 35 Yet another major review of risk factors identified risk factors from 63 studies which were grouped into two major categories. 25 The first category includes 22 risk factors related to conflicts or defects in the decision-making process , for example, feeling pressured to abort, conflicting maternal desires and moral beliefs, and inadequate pre-abortion counseling. The second category contains 25 risk factors related to psychological or developmental limitations , such as pre-existing mental health issues, lack of social support, and prior pregnancy loss. 25
The ability to identify women who are at greater risk of negative reactions has resulted in numerous recommendations for abortion providers to screen for these risk factors in order to provide additional counseling both before an abortion, including decision-making counseling, and after an abortion. 24 , 25 , 31 , 66 – 68
Notably, while there is no dispute regarding the abundance of research identifying risk factors, there is little if any research identifying which women, if any, acquire any mental health benefits from abortion compared to carrying a pregnancy to term, even if the pregnancy was unintended or unwanted. 17
All AMH studies have inherent limitations
It is impossible to conduct randomized double-blind studies to investigate abortion-associated outcomes. Such studies would require random selection of women to have abortions.
Notably, the very same fact that would make such a study unethical—forcing a group of women to have abortions—actually occurs in the real world wherein some women feel pressured or even forced into unwanted abortions by their partners, parents, employers, doctors, or other significant persons. 25 , 45 This problem with coerced abortions highlights one of the major difficulties involved in AMH research: any sample based entirely on self-selection (voluntary participation) no longer represents the full population of women actually having abortions. Indeed, since feeling pressured to abort is a major risk factor, the practice of excluding women aborting intended pregnancies from AMH studies 39 , 69 makes the results from such studies less generalizable to the actual population of all women having abortions.
This is just one of many difficulties which makes it truly impossible to conduct any AMH study that does not have significant methodological weaknesses. As a result, the “true prevalence” and intensity of the negative effects associated with abortion can never be known with any great certainty. Noting this problem, the TFMHA review concurred with the view that the complexity of this field “raises the question of whether empirical science is capable of informing understanding of the mental health implications of and public policy related to abortion,” admitting that many research “questions cannot be definitively answered through empirical research because they are not pragmatically or ethically possible.” 4
Despite study limitations, statistically significant risks are regularly identified
While every observational study can be criticized for methodological weaknesses, it is also nonetheless true that is still possible to discover meaningful and actionable results. For example, research demonstrating elevated rates of mental health problems among women who feel pressured to abort contrary to their moral beliefs is generalizable to that specific subset of women. So while it is important to never generalize to all women who have abortions, insights can be gained from nearly any study when the results are properly narrowed to the limits of the population studied. 70
Figure 1 shows the odds ratios (ORs) and 95% confidence interval (95% CI) for risks associated with abortion in all major studies published since 1995 organized by class of symptoms. 17 , 30 , 67 , 69 , 71 – 102
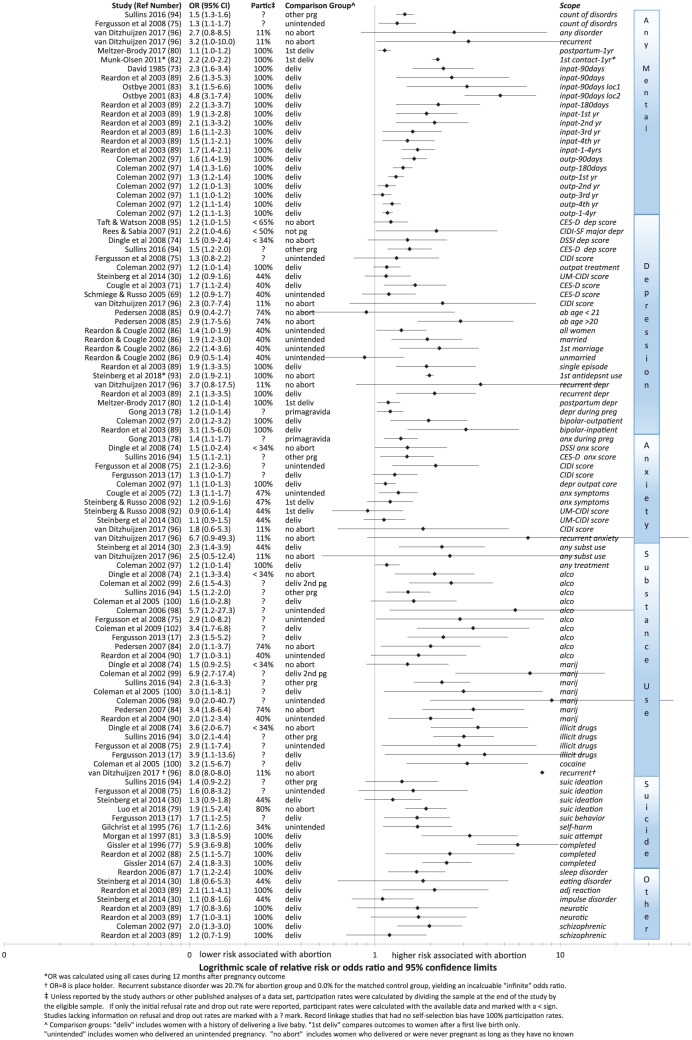
Relative risk of abortion relative to each study’s comparison groups.
While there are disagreements on how to best interpret these findings (to be discussed later), the findings themselves are not disputed. The results are organized into six sets: all classes of symptoms (segregated by inpatient and outpatient treatments when separately reported); depression and depression-related symptoms such as bipolar disorder; anxiety; substance use disorders (segregated by type of substance use when identified); and other disorders. Each row identifies the study reporting the results; the numeric relative risk (or OR) and CIs (also shown as a range in the forest plot); the participation rate of eligible women (after deducting refusals and dropouts) when identifiable; the group to whom the aborting women are being compared in the study; the forest plot; and an abbreviated description of the specific outcome, symptom, diagnostic scale, and/or time frame to which the statistic applies. Comparison groups include women carrying an unintended pregnancy to term, women delivering a child, women delivering a first pregnancy, women with no known history of abortion, women with any other pregnancy outcome other than abortion, and women not pregnant during the period studied.
What is most notable from Figure 1 is that the trend in results, including those reported by questionnaire and record linkage studies, is consistent. All but three odds ratios are above 1. In most cases, the lower 95% CI is also above 1, signifying statistical significance. Moreover, even among studies showing no significant difference (when the lower 95% CI is less than 1.0), the upper 95% CI is always above 1 and overlaps the statistically significant CIs of other studies.
This overlap is very important. For example, as can be seen in the depression grouping in Figure 1 , the overlap of the 95% CIs in the findings of Schmiege & Russo 2005 and Cougle 2003 (both using different sampling rules for the same data set) demonstrates that there is no actual contradiction in the findings of these two studies. Whenever there is overlap in the CIs, this tells us that the variation in the respective relative risks reported by each study is within the expected range of variation given the limits of each study’s statistical power. Since findings only contradict each other when there is no overlap in the CIs, it is clear from Figure 1 that the minority of studies without statistically significant findings do not contradict the findings of studies with statistically significant findings. Claims to the contrary 69 ignore the relevance of CIs and also the fact that studies with low statistical power are easily prone to Type II errors resulting in false negatives.
The risk of such false negatives is increased when there is also any risk of sample bias. In regard to abortion research, the risk of sample bias is especially high since questions about abortion are frequently associated with feelings of shame. 22 , 59 The resulting selection bias due to self-censure and the high dropout rates of women at greatest risk of negative reactions also contributes to the misclassification of women concealing a history of abortion as non-aborters. In addition, some researchers choose to exclude groups such as women who abort wanted pregnancies, 69 have later term abortions, or have other risk factors for more negative reactions ( Table 1 ) and these methodological choices will also tend to shift results below statistical significance.
Despite these problems, the trend in findings, as shown in Figure 1 , is very clear. Women who abort are at higher risk of many mental health problems.
This conclusion is strengthened by the variety of the study designs that have been conducted. Collectively, these studies examine a wide variety of different comparison groups, explore a diverse set of outcome variables, employ a large variety of control variables, and report on numerous outcomes over different time frames and/or at a variety of cross sections of time. Collectively, they reveal the following:
(a) There are no findings of mental health benefits associated with abortion. (These would be signified by the entire 95% confidence line being below 1.0.)
(b) The association between abortion and higher rates of anxiety, depression, substance use, traumatic symptoms, sleep disorders, and other negative outcomes is statistically significant in most analyses.
(c) The minority of analyses that do not show statistically significant higher rates of negative outcomes do not contradict those that do. (Shown by the upper bound of the 95% confidence overlapping the lower 95% CI of the statistically significant studies.)
A number of recent studies have also reported the population attributable risk (PAR) associated with abortion. This statistic estimates the percentage of an outcome that may be attributed to exposure to an abortion experience after statistically removing the effects associated with the available control variables.
Fergusson was the first to report PARs identified in a prospective longitudinal cohort studied from birth to 30 years of age in New Zealand. He reported that the attributable risk ranged from 1.5% to 5.5%, but did not identify the PAR of specific mental health effects nor provide the CIs. 75 Specific outcome PAR risks were also calculated by Coleman 15 in her meta-analysis, but these were reported without CIs. These are shown in Figure 2 along with PAR estimates with 95% CIs that have been reported in three other studies. 94 , 101 , 103
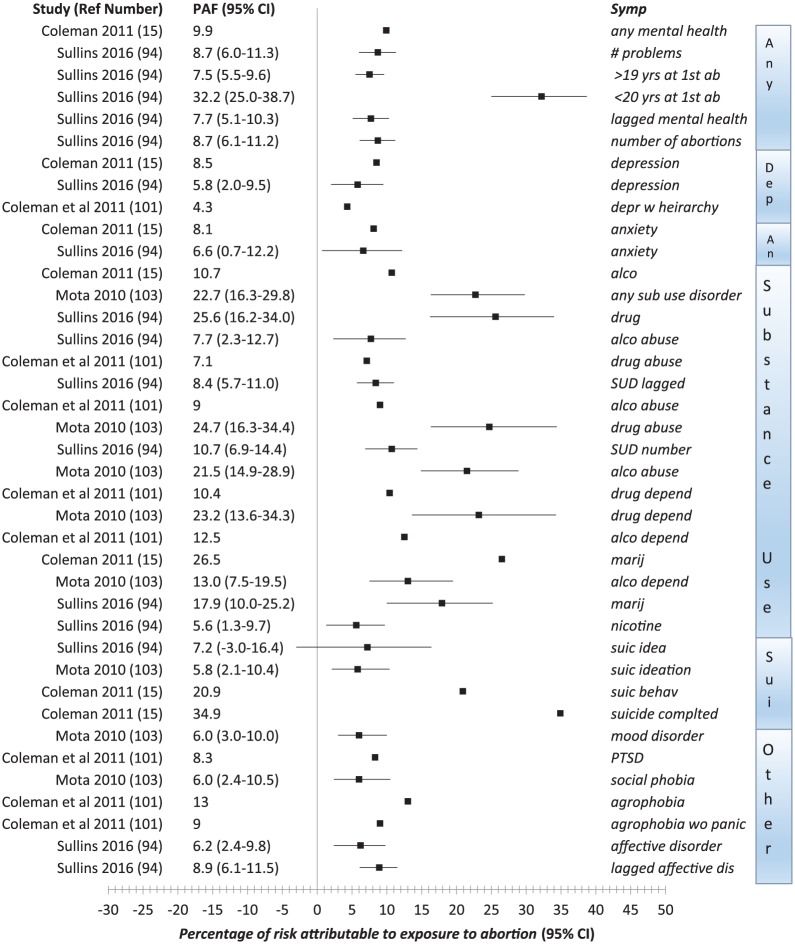
Population attributable fraction and 95% CI.
Of particular interest is a 2016 study by Sullins using the National Longitudinal Study of Adolescent to Adult Health that provided three models of analyses, including controls for 25 confounding factors. In addition, he conducted a fixed-effects regression analysis controlling for within-person variations to control “for all unobserved or unmeasured variance that may covary with abortion and/or mental health.” 94 Sullins’ lagged models, employed as additional means of examining effects of prior mental illness, confirmed that the risks associated with abortion cannot be fully explained by prior mental disorders. He also identified a dose effect, with each exposure to abortion (up to the four) associated with a 23 percent (95% CI, 1.16–1.30) increased of relative risk of subsequent mental disorders.
Collectively, the findings shown in Figure 2 suggest that substance use disorders appear to be most strongly attributable to abortion. Put another way, assessments of substance use (perhaps indicating self-medicating behavior) may be one of the more sensitive measures of difficulties adjusting to post-abortion. 96 Conversely, at least some research has shown that other outcomes, such as variations in self-esteem, may be unaffected, or only weakly associated with abortion. 38 Alternatively, some outcomes may appear to be less strongly associated with abortion because women are receiving successful treatment, such as medication for depression or anxiety, that would obviously suppress these associations with abortion.
Prior mental health and co-occurring factors explain at least part of the effects
As shown in Table 1 , a history of mental health problems is a risk factor for higher rates of mental health problems following abortion as compared to women without a history of mental health problems. This association has been known since at least 1973 when a case series identified several pre-existing mental health factors that could be used to identify the women who were most likely to experience subsequent psychopathology. 32 The authors of that study recommended that a low-cost computer scored Minnesota Multiphasic Personality Inventory assessment could effectively identify women who could benefit from additional pre- and post-abortion counseling.
Both AMH proponents and AMH minimalists agree that prior health is a major factor in explaining the negative reactions observed post-abortion. There are differences, however, in how proponents and minimalists distinguish, interpret, and emphasize the interactions between prior mental health, the abortion experience, and subsequent mental health.
AMH proponents see poor prior mental health as contributing to the risk that a woman (a) may become pregnant in problematic circumstances; (b) may be more vulnerable to pressure or manipulation to have an abortion contrary to personal preference, maternal desires, or moral ideals; and (c) may have fewer or weakened coping skills with which to process post-abortion stresses. In addition, from the perspective of abortion as a potential stressor, women exposed to prior traumatic experiences may be more predisposed to experiencing abortion as another traumatic experience.
In contrast, AMH minimalists tend to interpret the evidence that a high percentage of women having abortions have prior mental health issues as the primary explanation for higher rates of mental illness observed after abortion. 5 , 7 , 104 , 105 From this perspective, women with mental health problems are more likely to engage in risk-taking behavior and to experience more problematic pregnancies and are more likely to choose abortion. It is also hypothesized that pregnant women with pre-existing mental health problems may be more inclined to choose abortion because they recognize that they are likely to fare worse if they deliver and try to raise an unplanned child. 106 , 107 The higher rates of mental health issues following abortion, therefore, may be mostly explained as just a continuation of pre-existing mental health problems rather than a direct and independent cause of mental illness. While a few minimalists suggest that the underlying cause of mental health problems observed after abortion can be entirely explained by prior mental health defects or co-occurring stressors, 30 , 82 I have been unable to find any researchers who have denied that abortion can contribute to mental health problems.
A closely related issue is that a history of being physically and/or sexually abused is a co-occurring risk factor for both mental health problems and abortion. 92 , 94 , 108 – 110 Obviously, both sides agree that trauma from prior abuse can harm mental health. Also, at least from the clinical perspective of AMH proponents treating women with a history of both abortion and abuse, a history of abuse may increase the vulnerability of women consenting to unwanted abortions.
The differences between AMH minimalists and proponents on these issues will be more thoroughly discussed later. At this point, it is sufficient to note that both sides agree that poor prior mental health is a major predictor of higher rates of mental health problems after an abortion. Moreover, both sides agree that there should be mental health screening of women seeking abortion 24 – 30 , 32 – 38 , 58 precisely because the “abortion care setting may be an important intervention point for mental health screening and referrals” 30 due to the higher concentration of women with previous and subsequent mental health issues. At the very least, a history of abortion is a useful marker for identifying women at greater risk of mental health problems and a corresponding elevated risk of a variety of related chronic illnesses 111 and reduced longevity. 112 , 113
A summary of agreements with difference in emphasis
Table 2 summarizes specific factual propositions to which the vast majority of both AMH minimalists and AMH proponents would agree. As indicated in the table, each side may typically emphasize some points over others and might underemphasize, reluctantly admit, or even evade discussion of some of these propositions. Still, while some may quibble over the exact formulation of any particular proposition in Table 2 , the underlying consensus relative to each proposition is easily discernible in the body of references by both sides cited in this review.
Variations in emphasis on conclusions generally shared by AMH minimalists and AMH proponents.
AMH: abortion and mental health.
In summary, the consensus of expert opinion, including that of both AMH proponents and minimalists, is that (a) a history of abortion is consistently associated with elevated rates of mental illness compared to women without a history of abortion; (b) the abortion experience can directly contribute to mental health problems in some women; (c) there are risk factors, including pre-existing vulnerability to mental illness, which can be used to identify the women who are at greatest risk of mental health problems following an abortion; and (d) it is impossible to conduct research in this field in a manner that can definitively identify the extent of any mental illnesses following abortion, much less than the proportion of disorders that can be reliably attributed solely to abortion itself.
Obstacles in the way of research, understanding, and consensus
Facts are facts. But there is plenty of room for disagreement regarding which facts are generalizable, much less on how to best synthesize and interpret sets of facts, especially when there are flaws in the research and gaps in what one would want to know. Indeed, the greater the ideological differences between people regarding any question, the easier it is to disagree about what the available evidence really means. As shown in Table 2 , even areas around which there is a fundamental agreement by experts under sworn testimony may appear muddied by shifts of emphasis and the insertion of nuances that may be technically true but misleading to non-experts who imagine there are simple, global answers.
For example, the same APA task force which produced the list of risk factors shown in Table 1 did not highlight these findings in their press releases with a recommendation for screening. Instead, the centerpiece of their press release 114 was the report’s conclusion that “the relative risk of mental health problems among adult women who have a single , legal, first-trimester abortion of an unwanted pregnancy for nontherapeutic reasons is no greater than the risk among women who deliver an unwanted pregnancy” 7 (italics added).
This statement was widely reported as the APA officially concluding that abortion has no mental health risks. But as shown in Table 1 , this reassuring conclusion was actually couched in nuances which make it applicable to only a minority of women undergoing abortions on any given day. It excludes the 48%–52% of women who already have a history of one or more abortions, 64 the 18% of abortion patients who are minors, 115 the 11% of patients beyond the first trimester, 116 the 7% aborting for therapeutic reasons regarding their own health or concerns about the health of the fetus, 117 and the 11%–64% whose pregnancies are wanted, were planned, or for which women developed an attachment despite their problematic circumstances. 38 , 50 , 51
The above example demonstrates that the same set of facts, presented and interpreted by AMH minimalists in a way that suggests that few women face any risk of negative reactions to abortion, could also have been worded by AMH proponents in a way that would have underscored a conclusion that most women having abortions are at greater risk compared to the minority who have no risk factors.
This points to one of the greatest hindrances in the advance of knowledge: the tendency to use nuances to dodge direct engagement with the ideas, evidence, and arguments which threaten one’s own preconceptions.
Therefore, one of the purposes of the following discussion is to invite direct engagement and thoughtful responses to the specific obstacles identified below.
Intrinsic biases in the assessment of evidence are nearly impossible to avoid
Everyone, even the most “objective” scholar, has developed shortcuts in their thinking and beliefs. These shortcuts (or biases) help us to (a) be more efficient in drawing conclusions and making decisions and also (b) be more consistent in how we perceive ourselves and reality, or conversely, to avoid the stress of cognitive dissonance which occurs when some fact or experience clashes with our core beliefs and values.
Our biases are not just personal. They also have a communal element. We tend to adopt the biases of our peers for several practical reasons. First, by adopting the opinion of our peers as our own, we are embracing a collective wisdom that frees us from the need to deeply research and consider every idea on our own. Second, the more completely our beliefs are aligned within our community of peers, the less we will face conflict and suspicion. Obviously, there is never perfect alignment or cessation of independent thinking. But the tendency to accept the “conventional truths” of one’s peers as “fact” is a very real phenomenon.
The impact of biases among academics on the interpretation of data and suppression of contrary opinions has been well documented. 118 – 123 For example, identical studies, for which the results are the only difference, are more likely to be lauded or condemned 122 – 125 by peer reviewers when the results confirm or conflict with the reviewer’s own biases. In the fields of psychology and psychiatry, such confirmatory bias may contribute to the promotion or suppression of research findings that favor liberal causes. 125 – 128 In one study, only one-fourth of reviewers noted a major methodological problem in a fake study that agreed with their preconceptions, while 72% quickly raised an objection about the problem when presented with a nearly identical fake study in which the results challenged their preconceptions. 123 The only way to eliminate result-based bias, the author suggests, would be to solicit reviews only on the relevance of a study’s methodology, withholding the actual results and discussion of results, since the latter are the actual drivers of confirmatory bias. 123
While much of the confirmatory bias observed in peer reviewers may be unconscious, 129 at least one survey of 800 research psychologists found high rates of admissions that they or their colleagues would openly and knowingly discriminate against conservative views when providing peer review (34.2%), awarding grants (37.9%), or making hiring decisions (44.1%). 130 The authors noted that this admission of conscious ideological bias was likely just the tip of the iceberg compared to confirmatory bias since “[i]t is easier to detect bias in materials that oppose one’s beliefs than in material that supports it. 124 Work that supports liberal politics may thus seem unremarkable, whereas work that supports conservatism is seen as improperly ideological.” 130
In addition to blocking publication of good research, ideological and confirmatory bias may also contribute to poorly designed studies and/or carelessly interpreted findings that advance a preferred viewpoint. 118 , 126 , 131 – 133
Social psychologist Jonathan Haidt, a self-proclaimed liberal specializing in the foundations of morality and ideology, has argued that that the vast majority of psychologists are united by the “sacred values” of a “tribal-moral community” which is politically aligned with the liberal left. 134 This shared moral superiority, 129 he says, both “binds and blinds” their community. 134 The risk of “blindness” occurs because the lack of sufficient political diversity predisposes the community of psychologists to “embrace science whenever it supports their sacred values, but they’ll ditch it or distort it as soon as it threatens a sacred value.” 134
In regard to the abortion, mental health controversy, studies by AMH minimalists tend to be written in a way that minimizes any disruption of the core pro-choice aspiration that abortion is a civil right that advances the welfare of women. 135 The research on confirmatory bias discussed above, therefore, suggests that studies by AMH proponents are more likely to be unfavorably reviewed and rejected. 136
An excellent example of this result-based bias was the four rejections reported by David Fergusson, former director of the Christchurch Health and Development Study, which followed 1265 children born in Christchurch, New Zealand, for over 30 years. 137 Fergusson, a self-proclaimed pro-choice atheist, believed that his data would help to prove that AMH proponents were wrong. 137 But when he ran his analyses, he found that even after controlling for numerous factors, abortion was indeed independently associated with a two-to threefold increased risk of depression, anxiety, suicidal behaviors, and substance abuse disorders. 17 , 138 Though his findings were opposite to his preconceptions, he submitted them for pubication anyway. It was then that he ran into a wall of ideologically driven rejections and was even asked by the New Zealand government’s Abortion Supervisory Committee to withhold the results. 137
Similarly, Ann Speckhard, 139 another pro-choice AMH proponent and an associate professor of psychiatry at Georgetown University Medical School, has complained,
Politics have also stood in the way of good research being conducted to examine psychological responses in a nationally representative sample to all pregnancy outcomes: live birth, miscarriage, induced abortion, and stillbirth (and perhaps even including adoption). I offered in 1987 to our National Center for Health Statistics a simple mechanism for collecting such data via a short interview to be attached to an already existing survey—but fear of the answers—on both sides of the issue staunchly squelched the idea.
The problem is that even trained scientists struggle with being purely objective—especially regarding issues that may touch one’s own core beliefs, values, and experiences. What makes Fergusson’s experience particularly unique is that he chose to publish his findings even though they contradicted his own worldview. How many other researchers, expecting to prove mental health benefits from abortion but finding the opposite, might be tempted to withhold their findings, or worse, to redesign their study in ways that would obfuscate their results in order to declare that a lack of statistically significant results “proved” that there was no need to look further? This concern is heightened by the refusal of AMH minimalists to allow examination of their data by AMH proponents, 140 as will be discussed in more detail later.
Just as lawyers are taught to never ask a question at trial to which you do not already know the answer, researchers engaged in any field where there are “adversarial” positions may often be hesitant to cooperate in a mutual pursuit of objective truth. 141 This fear of admitting the validity of “the other side’s” concerns is also reflected in the admission by pro-choice feminists that they are afraid to publicize the existence of their own post-abortion counseling programs. 44 , 142
These concerns regarding bias surrounding AMH issues are further heightened by the fact that many professional organizations, including the APA, have taken official political positions defending abortion as a “civil right.” 135 In defense of that political position, Nancy Russo, a member of the APA’s TFMHA, has stated that “whether or not an abortion creates psychological difficulties is not relevant” 143 and has been a proponent of the APA taking a pro-active role in aggressively attacking the credibility of studies by AMH proponents. 144 The problem with professional organizations taking a political position on abortion is that any subsequent acknowledgment of negative mental health effects linked to abortion might then embarrass the APA, and/or other professional organizations that have committed themselves to the agenda of defending abortion as a civil right, and thereby creates an ideological obstacle in objectively evaluating new evidence.
There are different rates of exposure to the highest risk and lowest risk archetypes
This leads us to an important and perhaps closely related observation. It is not only political, philosophical, or ideological beliefs that contribute to the AMH controversy. Conflicts in the perceiving AMH controversy are also colored by direct and indirect personal experiences . The fact that pro-choice feminists are more focused on feelings of relief and other liberating aspects of having a right to abortion 3 may be accurately representing their own positive personal experiences. Conversely, anti-abortion conservatives, who presume that AMH problems are common, may be accurately representing their own relative rate of exposure to negative experiences. 3
Support for this hypothesis is found in a study based on structured interviews of women following their abortions conducted by Mary Zimmerman 48 in which she found that approximately half of the women she interviewed could be classified as “affiliated” (more goal oriented, more educated, less dependent on the approval of others, and more likely to abort for their own self-interest) and the other half as “disaffiliated” (less career oriented, less educated, more dependent on the approval of others, and more likely to abort to please others). When she interviewed her sample 6 weeks after their abortions, Zimmerman 48 found that only 26% of “affiliated” women were struggling with “troubled thoughts” about their abortions compared to 74% of “disaffiliated” women, a threefold increase. A similar disparity relative to personality types was observed by Major et al. 145
It is reasonable to assume that friends and associates of highly educated research psychologists are more likely to be skewed toward the “affiliated” than the “disaffiliated.” If so, the personal experience of such AMH skeptics may be dominated by the observation that they and their closest friends have generally coped well with any exposure to abortions.
Conversely, AMH proponents, especially those who directly meet and counsel women having problems dealing with past abortion 45 may have little or no experience with women who have had positive abortion experiences. The concentrated experience of meeting with scores or hundreds of women struggling with past abortions would understandably incline AMH proponents to believe that negative experiences with abortion are more common than positive ones. 146
In short, applying the general rule that people (including scientists) tend to look for and believe data that confirm their preconceptions, and are disproportionately skeptical of data that conflict with their preconceptions, both AMH skeptics and AMH proponents are at risk of preferentially interpreting their personal exposure to abortion’s risks and benefits as applicable to the general population.
While women having abortions will fall across the entire spectrum of risk factors, it is useful for this review to consider two hypothetical women at opposite ends of any risk-benefits analysis: (a) “Allie All-Risks,” the worst possible candidate for an abortion and (b) “Betsy Best-Case,” with no known risk factors:
“Allie All-Risks” is 15 years old. A victim of verbal, emotional, and physical abuse, including three incidents of sexual molestation, she has low self-esteem with bouts of anxiety, depression, and suicidal ideation. While her parents are not regular churchgoers, she attended a Catholic grade school, believes in God, and believes abortion is the killing of a baby. She is not a good student and has no concrete career goals. She has always wanted to be a mother, loves babies, and fantasizes about how she will find fulfillment in giving the love to her children that she never received from her own mother. Given Allie’s yearnings for escape, acceptance, and true love, she is vulnerable to the seductions of a 22-year-old womanizer with whom she falls madly in love and aspires to a happy future. When she learns she is pregnant, her initial reaction is excitement. While not planned, the pregnancy is welcomed. She believes she can now start building a family with her lover. But this fantasy is immediately crushed when he tells her that they can’t afford it, that neither of them are ready for it, and that if she decides to continue the pregnancy, he will leave her. She feels she has no choice. She can’t imagine losing him. In addition, her parents would be furious and insist on an abortion, too. Allie’s initial excitement at being pregnant is replaced by despair. Indeed, given her need to please others, she gives in with barely a complaint. Her mild protests about “their choice” go unnoticed. The day of the abortion she whispers: “Good bye. I don’t want to do this to you. But I don’t have a choice.” Immediately after the abortion, Allie feels a mild relief that the dreaded procedure is now behind her and hopes her boyfriend will be content, but alongside that relief are feelings of emptiness and loss that seem to grow stronger with every passing week. She begins to have obsessive thoughts. Her baby is no longer in her body, but it is constantly in her thoughts.
“Betsy Best-Case” is 32 years old. She has no history of mental illness and has a good family life. Her parents were both well-educated secularists. They preach education, hard work, and honest success as the only ethical standards Betsy needs to guide her. Betsy is popular, has many friends, and has always had high career aspirations, toward which, with grit, she has proudly made good progress. Even as a child, Betsy had little or no interest in being a mother. Married to her career, she now has even less interest in maternity. Having successfully used birth control since she was 15, when her mother got her an IUD, Betsy is shocked when she realizes she is pregnant. But contraceptive failures happen. Her decision to abort is immediate and made without any emotional conflict. When she flips through the state mandated informed consent booklet given to her at the abortion clinic, the pictures of developing fetuses have no effect. Betsy has seen similar photos many times in the past. She has a strong philosophical belief, based on years of engagement in minor abortion debates, that the value of being a “person” is not based on biological features but rather on the development of a psychological, purpose-filled, self-actualized human being far beyond anything to which a 9-week-old fetus could yet lay claim. Betsy is not surprised when her abortion is completed without drama or even a tinge of angst. She thinks of it rarely. The only negative feelings ever associated with it come when she hears the right of women to choose abortion attacked by self-righteous busybodies who should know better.
Hopefully, any reader can see and respect that the Allie and Betsy’s abortion experiences are very different. One is focused on her loss and the other on how her abortion helped her to avoid any loss. Given these differences, it would be unfair to them try to interpret their abortion experiences from within a single ideological framework. Similarly, the women who reside at different places along the wide spectrum between the extreme poles of Allie and Betsy are also very different and unique.
We will employ Allie and Betsy in our discussion later in this review. But for now, let them simply stand as examples of why AMH skeptics may, from personal experience, presume that Betsy is “typical” of abortion patients, while AMH proponents may presume that Allie is more “typical.” This difference in regard to how each side of the AMH controversy views the “typical” abortion patient is likely to impact how they interpret AMH research in their efforts to describe the experience of “most” women.
There are multiple pathways for AMH risks
Despite the convenience of standard diagnostic criteria, mental illnesses do not necessarily fit into neat, single classifications with distinct and exclusive symptoms arising from a single cause for each illness. 147 As noted in one review of the psychiatric complications of abortion,
A psychiatric complication is a disturbance that occurs as an outcome that is precipitated or at least favored by a previous event …. Every psychiatric outcome is of a multi-factorial origin. Predisposing factors including polygenic influence and precipitating factors such as stressful events are involved in this outcome; in addition, there are modulating, both risk and protective, factors. The impact of the events depends on how they are perceived, on psychological defense mechanisms put into action (unconscious to a great extent) and on the coping style. 18 (Emphasis added)
An abortion does not occur in isolation from interrelated personal, familial, and social conditions that influence the experience of becoming pregnant, the reaction to discovery of the pregnancy, and the abortion decision. These factors will also affect women’s post-abortion adjustments, including adjusting to the memory of the abortion itself, potential changes in relationships associated with the abortion, and whether this experience can be shared or must be kept secret. These are all parts of the abortion experience. Therefore, the mental health effects of abortion cannot be properly limited to the day on which the surgical or medical abortion takes place. The entirety of the abortion experience, including the weeks before and after it, must be considered.
Moreover, there is no reason to believe that there is a single model for understanding, much less predicting, all of the psychological reactions to the abortion experience. Miller alone identified and tested six models for interpreting psychological responses to abortion and concluded that
theoretical approaches that emphasize unitary affective responses to abortion, such as feelings of shame or guilt, loss or depression, and relief may be missing an important broader picture. To some extent what appears to happen following abortion involves not so much a unitary as a broad, multidimensional affective response. 148
The APA’s TFMHA proposed four models: (a) abortion as a traumatic experience, (b) abortion within a stress and coping perspective, (c) abortion within a socio-cultural context, and (d) abortion as associated with co-occurring risk factors. 7 Additional models could be built on biological responses, 149 , 150 attachment theory, 151 – 154 bereavement, 153 , 155 – 158 complicated, prolonged or impacted grief, 159 – 163 ambiguous loss, 156 , 161 , 164 – 167 or within a paradigm of psychological responses to miscarriage. 74 , 168 – 170
The complexity of considering so many models, or pathways, combined with the multiplicity of symptoms women attribute to their abortions, 45 contributes to discord in the literature produced by AMH proponents and AMH minimalists.
When there is no agreement on what outcomes are relevant or what theoretical pathways should be investigated, there are countless reasons to disagree about both (a) the adequacy of any specific studies and (b) how any specific set of findings should be best interpreted.
Women may simultaneously experience both positive and negative reactions
The act of undergoing an abortion can be both a stress reliever and a stress inducer. 171 It may relieve one’s immediate pressures and concerns while also leaving behind issues that may require attention immediately or at a future date. Positive and negative feelings can co-exist and frequently do. 38 , 39 , 48 , 50 , 166 , 172
In one study,
Almost one-half also had parallel feelings of guilt, as they regarded the abortion as a violation of their ethical values. The majority of the sample expressed relief while simultaneously experiencing the termination of the pregnancy as a loss coupled with feelings of grief/emptiness. 166
Another study found that 56% of women chose both positive and negative words to describe their upcoming abortion, 33% chose only negative words, and only 11% chose only positive words. 62 The women at greatest risk of experiencing negative reactions immediately and in the short term following an abortion are those who feel most conflicted about the decision to abort or have other pre-existing risk factors. 39 , 45 , 82 , 173
Applying this insight to our polar extremes, Annie All-Risks would be more likely to experience strong negative feelings more profoundly than her feelings of relief, whereas Betsy Best-Case would be more likely to focus on her relief than any doubts or reservations. Moreover, because Annie has low expectations for coping well (itself a TFMHA risk factor), she may be less likely to agree to participate in a follow-up study. The faster she can get out of the abortion clinic without talking to anyone, the better. Conversely, Betsy is confident that her decision is right and will improve her life and is therefore much more likely to participate.
What “most women” experience cannot be reliably measured
As will be further discussed later, the fact that positive and negative feelings can co-exist makes it difficult, and potentially misleading, to describe any single reaction to abortion as the “most common,” given the fact that (a) it is very rare for women to have a single reaction and (b) typically, over half of women asked to participate surveys regarding their abortion experiences refuse or drop out. Obviously, it is impossible to know what the most common reaction of women is based on surveys of only a minority of self-selected women.
This insight also underscores the difficulty of making any generalizations regarding prevalence rates from any study involving volunteer participation or questionnaires. Broadly speaking, there are three groups of women: (a) those with no regrets or negative feelings, (b) those with deep regrets and profound negative feelings, and (c) those with a mix of feelings, including contradictory feelings. As discussed above, the best evidence indicates that women with the most negative feelings are least likely to agree to participate in studies initiated at abortion clinics. But it also follows that women with no regrets are unlikely to be represented in studies of women seeking post-abortion counseling. Both of these factors underscore that it is impossible to accurately measure how “most” women react to their abortion experience when participation in research is voluntary.
The degree of reactions can widely vary and there is no reasonable cutoff for concern
Not all negative emotions constitute a diagnosable mental illness. Therefore, the fact that only a minority of women have diagnosable mental illnesses following abortion does not preclude the possibility that a majority experience negative emotional reactions.
Structured interviews of women who received abortions at participating clinics reveal that the majority report at least one negative emotion that they attribute to their abortions. 48 , 172 Given the relatively high rate of women refusing to participate in these follow-up studies, it is likely that the actual percentage of women having at least some negative reactions is well over half. 174 Similarly, retrospective questionnaires of women also reveal that over half attribute at least some negative reactions to their abortions. 50
The opinion that negative reactions are experienced by the majority of abortion patients is also shared by a number of abortion providers, such as Poppemna and Henderson: 175
Sorrow, quite apart from the sense of shame, is exhibited in some way by virtually every woman for whom I’ve performed an abortion, and that’s 20,000 as of 1995. The sorrow is revealed by the fact that most women cry at some point during the experience …. The grieving process may last from several days to several years.
Similarly, Julius Fogel, who as both a psychiatrist and OB-GYN and as a pioneer of abortion rights performed tens of thousands of abortion, testified that while abortion may be necessary and generally beneficial, it always exacts a psychological price:
Every woman—whatever her age, background or sexuality—has a trauma at destroying a pregnancy. A level of humanness is touched. This is a part of her own life. When she destroys a pregnancy, she is destroying herself. There is no way it can be innocuous. One is dealing with the life force. It is totally beside the point whether or not you think a life is there. You cannot deny that something is being created and that this creation is physically happening … Often the trauma may sink into the unconscious and never surface in the woman’s lifetime. But it is not as harmless and casual an event as many in the pro-abortion crowd insist. A psychological price is paid. It may be alienation; it may be a pushing away from human warmth, perhaps a hardening of the maternal instinct. Something happens on the deeper levels of a woman’s consciousness when she destroys a pregnancy. I know that as a psychiatrist. 176 , 177
This distinction between negative reactions and diagnosable mental illness is another important reason why AMH proponents and minimalists appear to disagree more than they really do. When AMH proponents make statements about “most women” which imply that negative reactions are common, they are including women who attribute any negative reactions to their abortions even if the reactions fall short of fitting a standard diagnosable illness. 45 Conversely, when AMH minimalists insist that “most women” do not experience mental illness due to their abortions, they are excluding the women who have negative feelings, even if unresolved and disturbing, on the grounds that (a) the symptoms do not rise above the threshold necessary to diagnose a clinically significant mental illness and (b) the symptoms cannot be strictly attributed to the abortion experience alone. 7
In short, if pressed, both sides would agree that the best evidence indicates that most women do experience at least some negative feelings related to their abortion experiences. Yet at the same time, the majority do not experience mental illnesses (as defined by standard diagnostic criteria) that can be solely attributed to their abortions.
This brings us to a more general problem regarding the claim that “the majority” of women experiencing relief following their abortions. 178 , 179 For women who do have strong negative feelings, such global denials of their personal experience may be demeaning. Even if these women’s negative reactions fall short of being classified as mental illnesses, it is reasonable for them to take offense at the AMH minimalist’s assertion that abortion does not involve any emotional risks, much less that the only women troubled by abortion are those who already had prior emotional problems. 180 In short, publicity suggesting that abortion has no psychological effects may have the unintended effect of making women who do struggle with a past abortion feel like “freaks” who are unable to handle their abortions as easily as “everyone else.” 45
Even if it could be proven that 99% of women who had abortions experienced more benefit than harm, that would still not justify ignoring the 1% who experienced more harm than good. Majorities matter in elections. But in regard to medical ethics and public policy, negative reactions are important among even a minority of patients … especially when it is possible to screen for risk factors that identify the patients at greatest risk of adverse reactions.
Negative reactions may manifest themselves over a very long time frame
Most studies can only capture evidence spanning very limited timeframes. In the 1960s and 1970s, most studies of emotional reactions after abortion were based on volunteer samples limited to a few hours, days, or weeks after the abortion. These studies typically found negative outcomes in the range of 10%–20% of their volunteer samples. Early reactions, however, are not necessarily predictive of longer range reactions. 38 Subsequent studies revealed that the percentage of women experiencing negative reactions increases with time, along with a significant drop in decision satisfaction and feelings of relief. 39 , 148
For example, in a study led by TFMHA chair Brenda Major, volunteers interviewed at an abortion clinic reported a significant decline in their Brief Symptom Inventory Depression scores 1–2 h after their abortions (T2, 62% decline) compared to their scores an hour before their abortions (T1, asking women to rate their depression for the month prior to the abortion). But at the 1-month follow-up (T3), depression scores rose 91% above their post-abortion (T2) score and continued to get higher, up to 118% at the 2-year follow-up (T4). 39 Notably, this study had a 30% dropout at the 1-month follow-up (T3) and a 50% dropout at the 2-year follow-up (T4). In addition, the self-selection bias of this volunteer sample was further magnified by the study protocol that also excluded women aborting an intended pregnancy or a second trimester pregnancy, two of the risk categories for elevated risk of negative reactions.
The fact that negative reactions may unfold over a long period of time is also evident from retrospective surveys. For example, one survey of women seeking post-abortion counseling found that only 24% claimed they had always been aware of negative feelings regarding their abortions. Of the remainder, less than half reported “doubts or negative feelings” within the first 3 years, while 100% were experiencing negative feelings by the time they sought post-abortion counseling. 45 A similar survey found that 70% of women seeking post-abortion counseling reported that there had been a time after their abortions when they would have denied having any negative feelings. 181 The first appearance of negative emotions may occur even as late as menopause. 182
It is likely that there are patterns relative to which women are at greater risk of experiencing early negative reactions and those who are likely to experience later reactions. Zimmerman, for example, found that 74% of “disaffiliated” women were struggling with negative thoughts about their abortions, three times the rate reported by “affiliated” women. 48 Thus, it is easy to predict that our archetype Annie All-Risks would likely be among those who would have immediate negative reactions. After all, she felt coerced into aborting an unplanned but welcomed pregnancy against her maternal preferences and moral beliefs. In addition, given her history of abuse and psychological problems, her coping skills were already stretched to the limit prior to her abortion.
Similarly, it is also easy to imagine that Betsy Best-Case would cope well in the immediate hours, days, months, and even years after her abortion. She freely chose to abort a pregnancy that was both unintended and unwanted for rational reasons. She also had strong coping skills and could easily compartmentalize any “socially induced” doubts into the “deeper levels” of her consciousness.
Clinical experience indicates, however, that there is no certainty that Betsy will always remain symptom free. Subsequent reproductive events such as miscarriage, infertility, or even a wanted birth may unexpectedly trigger existential crises deeply intertwined with a nearly forgotten abortion experience. 24 , 37 , 40 , 45 Similarly, life events that trigger introspection such as the death of a loved one, or a later religious conversion, may trigger a redefinition of past choices and experiences in a way that may include obsessive guilt and self-condemnation. 45 An example of a “perfect decision” being reinterpreted as a woman’s worst decision is found in this posting at a post-abortion counseling site:
I had an abortion when I was 22 years old. Now it is haunting me. I think about it every day of my life. I have so much regret. I wish I could turn the clock and undo my mistakes. I am not coping. The guilt is too much. At that time the decision was perfect. But now it kills me day by day. Please help me. I don’t trust anyone with this secret.
AMH minimalists might reasonably argue that it is the subsequent trigger, the miscarriage, or religious conversion, that is the “true cause” of later distress. But efforts to apportion blame for the “true cause” of distress over a prior abortion simply disrespects the real experience of women who seek, desire, or need post-abortion counseling. Whatever the trigger, whatever the contributing factors, the internal turmoil over a past abortion is centered on, or at least intertwines with, the abortion and will not be resolved by pretending the abortion is not part of the problem.
Based on reports of clinical experience, we would hypothesize that delayed reactions are most frequently triggered by (a) subsequent reproductive experiences, including reproductive difficulties and (b) experiences that lead to introspection and reevaluation of one’s overall life course or moral integrity. 45 Conversely, the more risk factors that are present, especially feelings of coercion and attachment combined with weakened coping skills, are predictive of more immediate negative reactions.
The great variability in the time frame for negative reactions greatly complicates the interpretation of studies examining limited time frames, and even those covering long time frames but at infrequent intervals. For example, two studies examined Center for Epidemiological Studies depression scores (CES-D) collected by the National Longitudinal Study of Youth (NLSY) an average of 8 years after an abortion. 69 , 86 But the NLSY was not designed to study reproductive or mental health and had a very high concealment rate regarding past abortions. Moreover, the single year in which depression was evaluated in the NLSY could only provide a bit of cross-sectional information about the women surveyed. While the passage of time may have helped to identify some delayed reactions, it would also miss cases where women have gone through a healing or recovery process during the 8 years (on average) for which there was no data. Moreover, the NLSY’s single measure for current depression, the CES-D, did not account for women who were being successfully treated for depression with medication.
In short, questionnaires which lack abortion-specific retrospective questions such as “Did you ever experience significant negative feelings about a past abortion?” followed by questions regarding the timeline for each type of mental health outcome being studied 45 , 50 , 183 are simply capturing cross-sectional data. Cross-sectional data regarding current symptoms will simply miss symptoms that have ceased, either due to medication, counseling, or by the healing effects of time or a replacement pregnancy. It will also miss symptoms that may be delayed beyond the date of the assessment. As a result, data from general prospective studies like the NLSY simply cannot tell us anything about the “true prevalence rate” of depression associated with abortion.
The weakness of such general purpose prospective studies also explains why AMH proponents and AMH minimalists can look at the same data and come to different conclusions. For example, the first analysis of NLSY CES-D scores relative to women with a history of abortion found that depression was highest among married women with a history of abortion (OR = 1.92; 95% CI = 1.24–2.97) and among women in their first marriage in particular (OR = 2.23; 95% CI = 1.36–3.74). 184 Since CES-D scores did not significantly vary among unmarried women, the combined results for all women (OR = 1.39; 95% CI = 1.02–1.90) were barely significant. 184 The significance of marital status may indicate that abortion-related depression after an average of 8 years may be triggered by subsequent pregnancies in marriage. In any event, given the weakness of this data set, it was a trivial matter for AMH minimalists 69 to use different selection criteria, excluding a subgroup of women at greatest risk of negative reactions to abortion, in order to shift the lower 95% CI for all women below 1 (OR = 1.19; 95% CI: 0.85–1.66) in their reanalysis of the NLSY data. Notably, their analysis also excluded results segregated by marital status, the finding most significant in the earlier study. Based on these weaknesses, it was simply misleading for Schmiege and Russo 69 to interpret their reanalysis as conclusive evidence that abortion does not contribute to the risk of depression in some women. Their overreaching conclusions were particularly unjustified in light of the fact that the NLSY data set was also tainted with a 60% concealment rate regarding past abortions 185 and the CES-D scale inquired about only depression in the prior week and was administered in only once, an average of 8 years after the abortions.
In summary, the efforts to estimate the prevalence rate of negative reactions to abortion are complicated by (a) the wide variety of reactions, (b) the existence of both early and delayed reactions, (c) a wide variety of triggers for delayed reactions, and (d) the prospect that in any assessment years after the abortion, a number of women who previously had significant reactions may have experienced full or partial recovery by the time of that assessment. Each of these factors would tend to skew the results of any prevalence estimates based on questionnaires toward underestimating the total lifetime risks.
Self-censure and defense mechanisms contribute to underreporting of sequelae
Data collected to investigate reactions to abortion may also be distorted by any number of defense mechanisms. Avoidance, denial, repression, suppression, intellectualization, rationalization, projection, splitting, and reaction formation may all contribute to the conscious or unconscious underreporting of symptoms attributable to unresolved abortion issues.
Active defense mechanisms are also the most likely explanation for selection bias and the high rate of concealing abortion history found in national longitudinal studies. Typically, respondents will report under half, and as few as 30%, of the number of abortions expected compared to age-adjusted national data on abortion rates. 106 , 185 , 186
In case series studies, where women are first contacted while at the abortion provider and asked to participate in a follow-up evaluation, both the initial refusal and subsequent dropouts usually exceed 50%. 39 , 187 In the Turnaway study, for example, only 37.5% of women asked to participate agreed, and of those who agreed 15% immediately dropped out before the first baseline interview, approximately 8 days after the abortion. 179 The study continued with phone interviews every 6 months for 5 years. Women were rewarded with a US$50 gift card each time they completed an interview. But despite this motivation, by the end of the 3 years, only 27% of the eligible women were participating, and this dropped to only 18% at the 5-year assessment. 188 Given this high rate of self-censure, the researchers’ conclusion that “Women experienced decreasing emotional intensity over time, and the overwhelming majority of women felt that termination was the right decision for them over three years” 179 clearly overstates what the Turnaway data can actually reveal. Unfortunately, the authors’ overgeneralized conclusion inspired many newspaper headlines which definitively proclaimed that the overwhelming majority of women are glad they had their abortions. 178 , 189 But if the researchers’ conclusions had been more accurately narrowed to describe their actual pool of respondents, the abstract should have read, “Of the 27% of eligible women participating at a three year assessment, the overwhelming majority felt that termination was the right decision for them.” That single clarification would have helped even the most pro-choice reporter to recognize that the views of a self-selected minority of volunteers (27%) simply cannot tell us what the “majority of women” feel and think. What “most women” experience is simply unknown when the majority of women are refusing to share their thoughts and feelings at any given time.
Avoidance, and other defense mechanisms, clearly works. Research has shown that the subset of women who anticipate the most difficulty dealing well with their abortions are right; they do have higher rates of negative reactions. 56 It is therefore natural for women who anticipate more negative reactions to avoid follow-up surveys that may aggravate those negative feelings. Indeed, one reproductive history survey that included as the last query, “Answering this survey has been emotionally difficult or disturbing,” found that women admitting a history of abortion were significantly more likely to feel disturbed by participating in the survey. 183 This finding is especially important relative to research designs that rely on waves of multiple interviews over time. Clearly, women who feel more stress at one wave may be more likely to decline to participate again in subsequent waves.
These findings are consistent with studies showing that women refusing to participate in follow-up studies are likely at greater risk of negative reactions to their abortions. 174 , 190 While one study has asserted that the women dropping out are not significantly different than subjects retained, 39 this conclusion was based on demographic comparisons, not on comparison of the presence of risk factors that are more predictive of negative reactions. The authors’ refusal to allow reanalysis of their data 140 also diminishes the reliability of their conclusions.
Notably, the act of avoiding a post-abortion evaluation may itself be evidence of a post-traumatic stress response. A study of 246 employees exposed to an industrial explosion revealed that those employees who were most resistant to a psychological checkup following the explosion had the highest rates and most severe cases of PTSD. Without repetitive outreach and the leverage of an employer mandate for undergoing post-traumatic assessments, 42% of the PTSD cases would not have been identified, including 64% of the most severe PTSD cases. 191 In the subsequent clinical treatment of these subjects, the author noted that “In the clinical analysis of the psychological resistance [to the initial assessment] among the 26 subjects with high PTSS-30 scores, their resistance was mainly found to reflect avoidance behavior, withdrawal, and social isolation.” 191
Our understanding of defense mechanisms also suggests there may be cases where the denial of a link between abortion and abortion-specific symptoms is evidence of both avoidant behavior and an elevated risk of mental illness. It seems likely that defense mechanisms may contribute to a significant underreporting of negative reactions, especially in survey responses. Conversely, questionnaire-based reports may also lead to the exaggerated rating of some positive reactions due to splitting or reaction formation. In these cases, women trying to focus on the positive may respond in ways that may anticipate, or even inflate, the positive feelings they want to feel while “rounding down” negative reactions which they want to escape or deny.
The statistical impact of defense mechanisms is also double edged. First, self-censure, dropouts, and concealment of past abortions are all likely to suppress measurements of the prevalence rate of mental illnesses among those volunteers admitting to a past abortion. Second, comparison groups that include women who conceal their history of abortion (who are most likely to have AMH effects) are likely to have inflated prevalence rates for mental illness due to the misclassification of women with a history of abortion into the comparison group of women who, according to the study design, have not been exposed to abortion. 184 Both problems suggest that odd ratios and prevalence rates based on studies relying on voluntary self-reporting of abortions will most likely be skewed toward underestimating the true risks associated with abortion.
It is also worth noting that defense mechanisms may also impede the ability of women to receive good follow-up care. In a survey of women reporting that they sought post-abortion counseling from a psychologist, psychiatrist, social worker, or other professional counselor, 58% reported that the counseling was not helpful. 45 Many reported that their therapists simply refused to seriously consider abortions as significant. This phenomenon may be at least partially due to defense mechanisms employed by healthcare professional professionals themselves. Many therapists may have unresolved issues with their own history with abortions; others may be loath to reconsider the wisdom of their advice to previous patients, reassuring them that abortion was a good; still others may have ideological commitments to abortion rights which conflict with their ability to trust their patient’s self-assessments, and some may simply have an uncritical confidence in the widely spread, but exaggerated claim, that “there is no evidence that abortion has any mental health risks.” This is yet another reason why better research and training regarding how abortion may contribute to problems for “ at least some women ” is important to prepare healthcare workers to be more sensitive and open to providing informed care. 45
There is no perfect control group; yet all comparison groups provide insights
Since it is impossible to randomly assign women to different groups to be exposed to abortion or not, there are no true control groups in relation to abortion among humans. Given this limitation, comparisons to other groups of women who have not been exposed to abortion are the only option. While no comparison group is perfect, 192 – 194 nearly every comparison can be useful for teasing out patterns that may help to inform patients and caregivers regarding the many varieties of abortion experiences.
Comparisons have been made to each of the following: the general population of women, 77 , 195 women who have never been pregnant, 94 women with no reported history of abortion, 74 , 84 , 85 , 91 , 92 , 94 , 95 , 100 , 101 women giving birth, 30 , 69 , 71 – 73 , 75 – 77 , 81 , 83 , 86 – 90 , 94 , 97 – 99 , 102 women giving birth to a first pregnancy, 69 , 86 , 113 women having miscarriages or other involuntary losses, 81 , 88 , 91 , 94 , 195 – 197 women experiencing both births and pregnancy loss (abortions or miscarriages), 69 , 82 , 107 women giving birth to unintended pregnancies, 69 , 72 , 75 , 76 , 86 , 90 , 92 , 98 and women denied abortions. 179 , 198 Together, these findings show that women with a history of abortion are statistically more likely to experience significantly more mental health issues relative to every comparison group that has been examined.
Notably, most of these comparisons are based on general-purpose longitudinal cohort studies. As discussed previously, due to the temporal limits, cross-sectional data, self-selection bias, concealment, and the misclassification of women with an abortion history into the comparison groups, the results of these studies most certainly skew toward underestimating the true relative risks between the groups compared. Still, while every choice for a comparison group is imperfect, 192 , 193 below we will argue that there are valid insights that can be gained by every comparison. Acting on that premise, many researchers have chosen to simultaneously compare women who abort to multiple other groups whenever the data allow it. 72 , 88 , 92 , 94
By contrast, Charles et al., 6 have argued that the only “appropriate” comparison group for AMH studies is to women who have “unwanted deliveries.” But this argument is weak for three major reasons.
First, the efforts to define and evaluate what constitutes an “unintended” or “unwanted” pregnancy are themselves imprecise, rendering any study based on such a flawed definition imprecise. 15 , 199 Moreover, not intending to become pregnant at a particular time in one’s life is very different than not wanting a child. Indeed, over half of unintended pregnancies are carried to term, accounting for approximately 37% of all births. 200 Conversely, among women having abortions, the evidence suggests that between 30% and 63% of aborted pregnancies were intended, wanted, welcomed, or involved significant emotional attachment. 48 , 50 , 51 , 148 , 172 In short, both groups (women having abortions and women carrying unintended pregnancies to term) encompass a huge variation in intentionality, wantedness, and attachment to their pregnancies.
Second, as Romans 192 has convincingly argued, the differences in women who choose to carry an unintended pregnancy to term and those who abort are simply immeasurable. No conceivable comparison between the two groups can control for all the possible variations between them. Still, as both the TFMHA 4 and Fergusson et al. 193 have argued, even imperfect comparisons have and can continue to yield valuable insights regarding the differences between the women who cope well and those who cope poorly. While such findings cannot tell us what “most women” experience, they can tell us how different subgroups of women compare to each other. These findings are meaningful and actionable since they should be used to guide pre-abortion screening and counseling and post-abortion care 25 and for informed consent procedures. 23
Third, the argument for discounting studies that lack information on pregnancy intention appears to have been advanced primarily as an excuse to denigrate the majority of studies on AMH. This charge is supported by the fact the “quality scale” created by Charles et al. 6 required deducting two of the five possible quality points from any study using any control group other than women carrying unwanted pregnancies to term.
The highly biased and subjective application of Charles et al.’s quality scale is demonstrated by the fact that they rated studies published by AMH minimalists 69 , 92 , 201 using exactly the same national longitudinal data sets as AMH proponents 72 , 86 , 101 consistently higher in quality. Moreover, Charles et al.’s quality scale totally ignored the problem of high concealment, misclassification, and drop-out rates in the very same studies they rated as better. Thus, by ignoring issues related to selection bias, the Charles et al. contrived ranking scale identified just four studies as “very good”—even though three of these had concealment rates of 60% or higher, 185 and the fourth had a dropout rate of 65%. 76 Meanwhile, their skewed scale allowed them to rank as “poor” or “very poor” literally all record linkage studies, which by their nature have no concealment or selection bias , 81 , 87 , 89 , 97 , 196 even though these same studies revealed some of the strongest associations between AMH problems.
The fact that Charles et al.’s study quality scale was deliberately skewed to serve the AMH minimalists’ perspective is perhaps best demonstrated by the fact that when the very same record linkage studies rated as poor by Charles et al. are rated using the Newcastle-Ottawa Quality Assessment Scale (NOQAS) for cohort studies, 202 a standard and widely used assessment tool across all disciplines, all receive very high scores, 8 or 9, on the NOQAS 9-point scale for quality. 203
In response to Charles et al.’s argument that the only appropriate comparison group is to women carrying unintended pregnancies to term, the following arguments are made in defense of other comparison groups. I argue that, while no comparison is perfect, every option for a comparison group can be a useful tool in developing a multidimensional perspective on the complexity of AMH issues.
First, comparisons to women with a history of abortion and the general population of women provide a useful baseline, especially when combined with comparisons to women who miscarry or carry to term. For example, a record linkage in Finland revealed that the age-adjusted risk of death within a year of pregnancy outcome was 5.5 per 100,000 deliveries, 16.5 per 100,000 miscarriages, and 33.8 per 100,000 abortions, compared to 11.8 per 100,000 age-adjusted women years for the general population of women not pregnant in the prior year. 196 A similar record linkage study of the population of Denmark revealed a dose effect, with the risk of death increasing by 45%, 114%, and 191% with exposure to one, two, or three abortions, respectively. 112 Yet another record linkage study examining attempted suicide rates before and after pregnancies revealed declining rates of suicide attempts after both delivery and miscarriage, but a sharp increase in attempted suicide following abortion, as seen in Figure 3 . 81
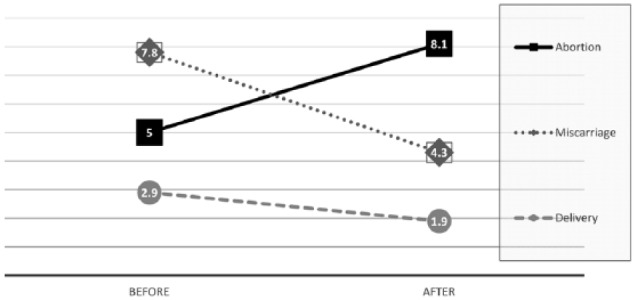
Suicide attempt rates per 100,000 women before and after designated pregnancy outcome.
Source: Morgan et al. 81
Comparisons to women who have never been pregnant (nulligravida) are especially important when the aborting women have no live born children. 74 , 92 , 94 , 113 , 204 Indeed, this is an important comparison since an abortion of a first pregnancy is essentially an effort to return a woman to her never been pregnant state. Differences between childless women with a history of one or more abortions and those without any history of pregnancy may provide valuable insights into the effects of an interrupted pregnancy on women’s emotional and physical health.
Another important comparison is between women who have induced abortions and women who miscarry. Both have experienced the effects of pregnancy, which may produce long-lasting changes to the brain, 150 , 205 , 206 and maternal attachment. 151 , 152 , 154 , 207 While the physiological processes of natural miscarriage and induced abortion are different, there may be similarities in the recovery process. Moreover, this comparison may allow insights into the psychological differences between intentionally choosing the end of a pregnancy versus an unintended loss, both of which may be experienced as a form of disenfranchised grief. 45 , 161 Arguably, examining the differences between miscarriage and abortion may be the most relevant and important comparison. 203
Comparisons to women giving birth are also meaningful. Just as a comparison to a never pregnant woman attempts to estimate how closely induced abortion achieves the goal of “turning back the clock” to the point before the woman became pregnant, a comparison to a delivering woman seeks to estimate how a woman’s mental health would fare if she chooses to “move into” the group of women giving birth.
Comparisons between women aborting a first pregnancy and women carrying a first pregnancy to its natural conclusion (birth, miscarriage, or neo-natal loss) are extremely valuable. By excluding the confounding effects of multiple pregnancy outcomes, these studies offer at least a small window on the effects associated with exposure to a single pregnancy outcome. Moreover, they are the proper starting point for investigating the interactions between multiple pregnancy outcomes. This is important since significantly different outcome patterns have been observed relative to multiple pregnancy outcomes and their sequences, including both multiple losses and losses followed or preceded by live births. 88 , 94
While comparisons of first pregnancy outcomes are valuable, it should be noted that it is a very poor methodological choice to include in the group of women experiencing a “first live birth” women who are known to have had one or more abortions before their first live birth or between the birth and the date of the mental health assessment. 69 , 107 Unfortunately, these flawed studies 69 , 82 , 107 , 208 – 210 ignore the extensive evidence showing that a history of pregnancy loss (abortion or miscarriage) is associated with higher rates of mental health problems during subsequent pregnancies. 78 , 80 , 99 , 100 , 170 , 211 – 226 By adulterating the “control” group of women having a “first live birth” with women who also have a history of one or more abortion and/or miscarriages, the resulting analyses clearly confound rather than clarify the differences between abortion, miscarriage, and childbirth, shifting the known negative effects associated with prior pregnancy losses into results associated with a first childbirth. 69 , 82 , 107 , 208 – 210 Arguably, this confounding methodology has been specifically employed by AMH minimalists precisely with the intent of producing results that obfuscate the mental health effects associated with abortion while inflating the effects associated with childbirth. 141 , 227
As will be discussed further, we recommend that the best practice for all studies examining the interactions between mental and reproductive health is to include stratification of results by the order and number of exposures to births, abortions, miscarriages, and other pregnancy losses. 94 , 141 , 227 Otherwise, the effects of different pregnancy outcomes are likely to be obscured rather than clarified.
In addition, we would note that the argument of Charles et al. for discounting studies that lack controls for pregnancy intention may do a major disservice to both women considering abortion and their caregivers. For all the reasons given above, the best evidence indicates that reasonable patients may consider any and all of the comparisons discussed above to be of value in their efforts to evaluate the potential risks and benefits of an abortion in their own personal circumstance 23 , 25
Finally, it has been argued that the differences between women who abort and those who do not are so extreme that the only meaningful comparison is between women who abort and women who sought but were denied an abortion. 194 While this comparison might be informative, it is clearly not a perfect comparison since the reasons why women may end up being denied an abortion are also likely to make these women significantly different than the average woman seeking and obtaining an abortion. Moreover, since in most countries where abortion is legal, very few women are denied an abortion undertaking such studies may be impractical. Indeed, the only set data set using this control group is the so-called Turnaway Study. Indeed, the argument that this is the only valid comparison group appears to be made in an attempt to dismiss all other research in favor of this single data set. But there are many problems with the Turnaway Study data set. 198 The most damning is the problem of self-censure. Over 70% of women approached to participate in this study refused, even after they were promised payments for participating, plus, nearly half of those who did participate subsequently dropped out. 198 This high refusal rate alone renders the Turn-Away Study data meaningless in terms of drawing any conclusions regarding the general population of women seeking or having abortions, and that is just one of many major flaws in the Turnaway Study methodology and execution. 198
Poorly defined terms produce misleading conclusions: unwanted, relief, and more
Unfortunately, a great deal of the literature on AMH revolves around poorly defined terms. The resulting lack of precision and nuance contribute to AMH minimalists and AMH proponents talking past each other and contributes to overgeneralizations regarding research findings, especially in the press releases and position papers of pro-choice and anti-abortion activists.
As previously discussed, one common overgeneralization is the assertion that abortions typically involve “unwanted” pregnancies. A closer look, however, reveals that many aborted pregnancies, perhaps the majority, occur for planned, partially wanted, or initially welcomed pregnancies. 48 , 50 , 51 , 148 , 172 By “welcomed” pregnancies, I mean pregnancies which were not planned in advance but to which the woman was open or naturally inclined to accept and embrace if only she had received the support of her partner, family, or others. 45 , 181 , 228
Attempts to define “unwanted” pregnancies are also complicated by the fact that many women report a divide between their emotional and intellectual responses when they first discover they are pregnant. Emotionally, they may be excited that a new life is growing inside them and may fantasize about having the child. But at the same time, their logical side may be immediately convinced that abortion is their only pragmatic choice. 45 The pregnancy may therefore be simultaneously “emotionally wanted” and “logically unwanted.”
Based on both clinical experience and case series studies, 173 we hypothesize that many delayed reactions to abortion stem from the psychological conflicts that arise when emotions are suppressed in favor of pragmatic choices. In such cases, forward-looking women with strong defense mechanisms are likely to cope well with their choice for many years. But if this coping is achieved by suppressed emotions, this may consume energy and may even fuel maladaptive behaviors, like substance use and sleep disorders. Any connection between these symptoms and underlying abortion associated conflicts may not be recognized until some subsequent event or stress compels a reexamination of unresolved maternal attachments or the woman’s moral priorities.
One measure of openness to having a child, seldom addressed in AMH studies, is desire for children at some later date. A high level of desire for future children suggests that an aborted pregnancy was most likely problematic due to specific circumstance or lack of sufficient social support. Among a sample of women seeking counseling for post-abortion distress, 64% felt “forced by outside circumstance” to have an abortion and 83% indicated they would have carried to term if significant others in their lives had encouraged delivery. 181 While statistics gathered from women contacting post-abortion recovery programs may be not representative of the general population of women, these findings demonstrate that labeling these aborted pregnancies as “unwanted” does not reflect the experience of the women who subsequently do seek post-abortion help.
Given the wide variation in levels of intention or openness to pregnancy, much more extensive data on intention 199 , 228 and attachment 207 are required to draw any conclusions regarding the mental health effects of abortion relative to various levels of women’s attachment, intention, and outcome preferences.
A second poorly defined variable is “relief.” AMH minimalists have frequently asserted that the most common reaction to abortion is relief. 4 But “relief” is a very broad term. A woman reporting “relief” may be referring to (a) relief that she will not have a baby, (b) relief that a dreaded medical procedure is now behind her, (c) relief that her parents will not discover she was pregnant, (d) relief that her partner will finally stop harassing her to have an abortion, or (e) any number of other reasons for feeling a reduction in stress.
But as indicated earlier, abortion can be both a stress reliever and a stress creator. The many declarations by AMH minimalists that “relief” is the most common reaction to abortion tend to distract the public from the fact that the vast majority of women reporting relief are also reporting a host of negative feelings at the same time. 39 , 50 , 62
Similarly, claims that “the most common reaction” to abortion is relief is also misleading because it falsely suggests that a truly representative sample of all women having abortions have been queried about their most prominent and common reactions. But in fact, all the case series studies assessing “relief” have self-censure and dropout rates exceeding 50%. 39 , 59 When only a minority of women agree to report on their reactions to an abortion, these studies cannot reliably tell us anything about the majority of women. This is especially true if the self-selection bias is toward women who expect to feel more relief because their abortion decision is more consistent with their own desires and preferences, while those who refuse to participate anticipate and do experience more negative reactions. 174 , 190 , 191
Another misleading factor is that relief is most often reported as a single variable whereas negative reactions are often averaged together. For example, one of the most frequently cited case-series reporting that women felt “more relief than either positive or negative emotions” was based on comparing the results of a single question regarding relief to an average of six scores (“sad,” “disappointed,” “guilty,” “blue,” “low,” and “feelings of loss”) chosen to represent negative emotions and an average of three scores (“happy,” “pleased” and “satisfied”) chosen to represent positive emotions (excluding relief). 39 This methodology was highly problematic.
While it would be interesting to see score distributions for each reaction separately, 45 how can a variety of emotions be “averaged” together in any meaningful way? For example, if a score of 1 (corresponding to “not at all” on the Likert-type scale used) is equivalent to 0% of the relevant emotion and a 5 (“a great deal”) is 100% of that emotion, averaging six emotion scores together presumes that a rating of 3 (50%) for “disappointed” is truly equivalent to twice a rating of 2 (25%) for “feelings of loss” and half the value of a rating of 5 for “guilty.”
But what makes this averaging process even more suspect is that the least common negative reaction (“disappointed,” perhaps) would dilute the entire average of negative reactions, concealing the frequency of the more common reactions (“guilty,” perhaps). Most importantly, while the most common negative and positive reactions were diluted by this “averaging” process, the “relief” score was not subject to the dilution by averaging with any of the other positive emotions.
Yet another problem with the authors’ conclusion 39 was their presumption that the six negative reactions they asked about are actually the most common negative reactions. But three of the six negative reactions (“sad,” “blue,” “low”) appear nearly synonymous. The similarity of these three may have been deliberate in order to boost the reliability score for the authors’ scale. One of the remaining choices, “disappointed,” is simply odd, rather bland, and perhaps disinviting as it is not a term that has been reported in interviews with women reporting negative reactions to abortion. 45 , 172 , 173 , 181 While the assessments of “guilty” and “feelings of loss” were appropriate, it would have been more illuminating to report these separately rather than in an “average” of negative emotions.
In any event, averaging emotion scores is problematic and in this case the choice of the six negative feelings chosen to be averaged together failed to include many of the negative emotions most commonly reported in surveys of the women who seek post-abortion counseling, including sorrow, shame, remorse, emptiness, anger, loneliness, confusion, feigned happiness, loss of confidence, and despair. 45
Despite the many limitations regarding the claim that “relief” is more common than negative reactions, it is notable that the same researchers also found that between the 3-month and 2-year post-abortion assessments, both relief scores and positive emotions decreased significantly while the average for negative emotions increased. 39 In other words, even with a self-selected sample of women most likely to have more positive reactions, those positive emotions declined and negative emotions increased within the first 2 years. If that trend continued over 20 years, the finding that the “most common reaction” to abortion was relief may not have held up over a longer period of time.
Similar problems apply to the widely reported claim that most women are satisfied with their decisions to abort. 179 In this case, the self-selection bias was profound, with only 27% of the eligible women participating at the date of their first assessment. In addition, this “finding” was based on a binary yes or no response to a single question: “Given your situation, was your decision to have an abortion right for you?” This question clearly invited reaction formation and splitting. Additional questions, such as, “If you had received support from others, would you have preferred to have carried to term?” would have provided deeper insight into the participants’ true preferences.
Despite the problems with their methodology and self-selected sample, these researchers’ confident assertion that the vast majority of women are satisfied with their abortions generated bold headlines. 189 But these misleading headlines were clearly based on poor science. 198 Similar questions, posed to a different self-selected sample of women seeking post-abortion counseling, reveal that 98% of that sample of women regret their abortions. 45 These resuts are contradictoruy because neither of the two samples just cited represent the general population of women having abortions. Given the fact that so many women refuse to respond to questionnaires about their abortions, it is impossible to ever be certain what “the majority” of women feel or think about their past abortions at any given time, much less through their entire lifetimes.
If there is any consistency in the evidence, it is in regard to the finding that satisfaction declines and regrets increase over time. 38 , 39 , 45 Therefore, the existing data for claims regarding high levels of relief and decision satisfaction are highly questionable in the short term and meaningless in regard to predicting feelings in the long term.
Is abortion the sole cause, a contributing cause, or never a cause of mental health problems? Or is this question just a distraction from helping women?
Normally, the burden of proving that any proposed medical treatment produces real benefits which outweigh any risks associated with the procedure falls on the proponents of the treatment. 229 Indeed, proponents of a treatment are also tasked with the obligation of proving not only specific benefits but also with identifying the symptoms and circumstances for which the treatment has been proven to be beneficial and those cases for which it might be contraindicated. After all, no treatment is a panacea. Even highly successful elective treatments such as Lasik are contraindicated for 20%–30% of patients considering the surgery. 230
Evidence-based medicine is centered on the idea that there must be real evidence of benefits that outweigh the risks associated with a medical intervention. But there are no statistically validated medical studies showing that women facing any specific disease or fetal anomaly fare better if they have an abortion compared to similar women who allow the pregnancy to continue to a natural outcome. 17 , 231 , 232 Nor is there evidence of any mental health benefits. 17 , 25 As a result, in approaching a risk–benefits assessment, there are literally no studies to place in the benefits column of an evidence-based risk–benefits analysis. Conversely, there are literally hundreds of studies with statistically significant risks (both physical and mental) associated with abortion which must be considered in weighing abortion’s potential risks against the patient’s hoped for benefits. 11 , 112 , 113 , 232 , 233 See, for example, the references to Table 1 .
In this regard, induced abortion is an anomaly. It is the only medical treatment for which the principles of evidence-based medicine are routinely ignored, not for medical reasons, but by appeals to abortion being a fundamental civil right 135 or a public policy tool for population control. 25 From these vantage points, there has arisen an a priori premise that abortion should presumed to be safe and beneficial. Therefore, according to defenders of abortion, the burden of proving the safety and efficacy of abortion is no longer on them. Instead, abortion skeptics must prove that abortion is the sole and direct cause of harm to women—and not just a few unfortunate women, but a large proportion of women. 4 , 6 , 57
This difference in evaluating abortion compared to other medical treatments was at the center of a Planned Parenthood suit challenging a South Dakota statute requiring abortion providers to inform women of research regarding psychological risks associated with abortion. Abortion providers argued that there was not yet enough proof that abortion was the “direct cause” of the statistically significant higher risks of mental illness, including suicide, following abortion. Therefore, they argued, disclosing the findings of these studies to women might unnecessarily frighten their patients. 234 But the Eighth Circuit United States Federal Court of Appeals rejected Planned Parenthood’s argument, ruling that it was a standard practice in medicine to “recognize a strongly correlated adverse outcome as a ‘risk’, even while further studies are being conducted to investigate which factors play causal roles.” 234 The court went on to add that Planned Parenthood’s “contravention of that standard practice” had no legal merit since “there is no constitutional requirement to invert the traditional understanding of ‘risk’ by requiring, where abortion is involved, that conclusive understanding of causation be obtained first.” 234
This appellate court’s ruling is consistent with idea that “risk,” by definition, includes uncertainty—otherwise, it would not be a “risk” but rather a “certainty.” Therefore, the question of whether a statistically significant risk is solely due to abortion, partially due to abortion, or only incidentally associated with abortion is itself just another of the uncertainties about the procedure, and therefore a true risk about which patients should be informed. 25
The court’s decision favoring disclosure of all risks, even when causality is challenged by proponents of the procedure, is in line with the preferences reported by 95% of women considering elective medical procedures, to be informed of “all possible complications.” 23 From a feminist perspective, the right of each individual woman to evaluate for herself whether a statistically significant risk is incidental or causal would also appear be central to the protection of each woman’s personal liberty. Indeed, the United Nation’s Fourth World Conference on Women’s Declaration and Platform for Action, which specifically addressed the issue of unsafe abortions, urged every government to
Take all appropriate measures to eliminate harmful, medically unnecessary or coercive medical interventions, as well as inappropriate medication and over-medication of women, and ensure that all women are fully informed of their options, including likely benefits and potential side-effects, by properly trained personnel. 235 (Emphasis added)
For the reasons above, the claim that the higher incidence rates of mental health problems associated with abortion are most likely “spurious” 105 has no bearing on informed consent. Only after full disclosure can each patient judge the relevance of such information for herself.
These challenges are also irrelevant to the obligation of the treating clinician to screen for the risk factors associated with higher rates of negative outcomes associated with abortion. 23 , 25 After all, even if abortion proponents could prove that 100% of all the negative effects associated with abortion are causally due to common risk factors, the finding that abortion is consistently associated with higher rates of mental health problems 15 , 57 , 82 , 89 , 94 is still an actionable marker that can and should be used to identify women who may benefit from referrals for additional counseling. 26 , 27 , 30 , 32 – 34 , 36 – 39
Still, the question of causation is worthy of additional attention. One approach for judging causality is to apply the nine criteria Bradford-Hill proposed to identify the causal role that occupational and lifestyle factors may play in the development of diseases, such as cancer. These include temporal sequence, strength of association, consistency, specificity, biological gradient (dose–effect), biologic rationale, coherence, experimental evidence, and analogous evidence. 236 Applying the Bradford-Hill criteria to the AMH question, Fergusson, a pro-choice proponent, concluded that “the weight of the evidence favors the view that abortion has a small causal effect on the mental health problem.” 75
It should be noted, however, that the Bradford-Hill criteria were developed to evaluate contributing factors for physiological diseases. Bradford-Hill therefore ignored a type of evidence for causality which is unique to psychological diseases, namely, self-aware attribution of causal pathways. For example, the evidence of a woman who says, “After the death of my child, I drank more heavily to dull the pain,” is a conscious identification of cause and effect regarding her own mental state and behaviors.
Indeed, in the psychological sciences, it has been a traditional practice to begin any investigation of mental illness by first listening to those individuals who claim they have a psychological problem. After carefully listening to a “sick” population, psychologists can then map the range of reported symptoms and then build hypothesis regarding the contributing factors and causal pathways which can then be explored by surveys of the general population. This was the approach AMH proponents used in their initial investigations of women seeking post-abortion counseling. 45 , 171 , 181 Because these samples were based on women experiencing post-abortion issues, they were likely skewed toward the Allie All-Risks archetype. Still, because they were focused on developing a profile of the women having post-abortion issues, this was a valid starting point for identifying the most common complaints and recurring patterns.
By contrast, most AMH minimalists have tested their hypotheses using surveys of women contacted at abortion clinics. These survey instruments appear to have been developed with little or no attention to the complaints of the women who reported post-abortion mental health crises. Moreover, because these surveys are implemented in cooperation with abortion providers, in a stressful situation during which less than half of the women agree to participate, it is likely that these self-selected samples skew toward the Betsy Best-Case archetype. 39 , 237
Even though AMH minimalists and proponents approach their research from different perspectives, the results from both sides consistently show that at least a minority of women experience mental health problems that they attribute, at least in part, to their abortions. While not included in the Bradford-Hill criteria, when it comes to mental health issues, the fact that so many intelligent, self-aware women attribute specific patterns of emotional distress to their history of abortion is one of the strongest pieces of evidence that abortion directly contributes to mental health problems. The same is true with regard to mental health associated with miscarriage. The validity of this evidence is further strengthened by the professional assessment of both pro-choice therapists 40 – 44 and pro-life therapists 45 – 47 who also attest to the causal connection.
Similarly, the clinical evidence that women struggling with post-abortion mental health issues improve following treatment focused on their abortion loss 40 , 46 , 238 – 240 also supports the conclusion that abortion can cause, trigger, or exacerbate psychological illness. After all, a successful treatment is evidence in favor of a correct diagnosis.
As previously noted, self-attribution is not perfect evidence. Defense mechanisms often operate by obscuring the “true cause” of one’s mental distress. But we would argue that the bias of defense mechanisms would be toward underreporting of effects truly associated with an abortion rather than toward false attribution of unrelated effects to past abortions.
That is not to say that pre-existing mental health issues cannot become intermingled with an abortion. To the contrary, clinical experience shows that abortion can become such a significant stressor in a woman’s life that other pre-existing issues can become enmeshed in the abortion and its aftermath. Pre-existing substance abuse, for example, may become intensified in the abortion aftermath, but it would be a self-deception to blame the abortion entirely for such substance abuse. On the contrary, once the issues become intermeshed, progress in dealing with underlying issues will be hindered by a failure to address the intermingled abortion issues.
Similarly, even in cases where suicide notes specifically attribute a woman’s final act of despair to her recent abortion, 241 other pre-existing factors may also contribute to these tragedies. In short, while it would be absurd and insulting to deny that abortion at least contributes to such suicides, it would be a mistake to assume that abortion is the sole cause of suicide or any other specific mental illness.
As stated previously, abortion does not occur in isolation from interrelated personal, familial, and social conditions that influence the experience and mental health of each individual. Moreover, there are likely a multiplicity of different pathways for effects to manifest either in the near or longer term. 18 In general then, abortion is most likely a contributing factor to the manifestation of problems rather than the sole factor . It may be trigger latent issues, intensify or complicate existing issues, interact with pre-existing issues to create new issues, or contribute in any number of ways unique to any particular individual’s susceptibilities and prior and subsequent life stresses.
In summary, there is incontrovertible evidence that abortion contributes to mental health problems, both directly and indirectly. Based on reports of clinical experience, it would appear that abortion can be the primary cause for mental health issues in some women. But it may also trigger, intensify, prolong, or complicate pre-existing mental health issues. Still, for the sake of argument, assuming AMH minimalists are right in their assumption that abortion itself is never the “sole cause” of mental health problems, there is still no reasonable doubt that abortion contributes to mental health issues in some women.
Finally, it should be emphasized that the difficulties involved in proving causality cut both ways. The burden of proving the efficacy and safety of abortion falls on abortion providers. To date, they have failed to provide any evidence, much less proof, that abortion is the sole and direct cause of any health benefits for women in general, or even for specific subgroups of women. 193 , 232 Nor have they shown that the benefits women hope to obtain through abortion are proportionate to or greater than the significantly elevated rates of negative outcomes associated with abortion. In this regard, abortion continues to be an experimental treatment, one for which they hoped for benefits are unproven. And with no proven benefits, the risks–benefits ratio is unknown even for those women without any known risk factors.
Is it reasonable to attribute all negative effects to pre-existing factors?
There is no longer any dispute regarding the fact that, on average, women with a history of abortion have higher rates of mental illness compared to similar women without a history of abortion. But AMH minimalists frame this admission in the context of arguing that this is most likely due to pre-existing mental health issues. 5 , 6 , 242 In other words, they argue that a higher percentage of aborting women were “already emotionally broken” to begin with. Therefore, higher rates of mental illness following abortion are just a continuation of pre-existing mental frailty.
This argument is indistinguishable from the centuries-old accusation of personal defects applied to “hysterics,” “malingerers,” “cowards” and others who exhibit traumatic reactions. 45 , 243 This blame-their-weakness argument is just a corollary to the assertion that higher quality, more emotionally stable people simply do not break under such circumstances.
In courtrooms, this line of arguments is known as the thin skull, or eggshell skull, defense. It asserts that a defendant should not be held accountable for injuries that would not have been suffered if the plaintiff had not been predisposed to injury due to pre-existing physical or emotional defects. Notably, the thin skull defense has been rejected in most legal jurisdictions. Even if the damages of the “frail” plaintiff are greater than they would be for a healthier person, jurists have ruled, the defendant is still liable for the greater damages because
a defendant who negligently inflicts injury on another takes the injured party as he finds her , which means it is not a defense that some other person of greater strength, constitution, or emotional makeup might have been less injured, or differently injured, or quicker to recover. 244 (Emphasis added)
Applying the thin skull legal analysis to abortion, this means that a physician who fails to screen for known risk factors, such as prior mental illness, before recommending or performing an abortion is guilty of negligence if the woman suffers any subsequent mental health problems because it is precisely the obligation of the physician to treat the woman “as he finds her.”
In short, the argument that negative effects may be mostly due to pre-existing mental health problems simply strengthens the argument for better pre-abortion screening for this and other risk factors. 12 , 25 , 26 , 32 Conversely, it does not at all support the presumption that abortion is safe or likely beneficial to most women, much less all.
The “broken women” argument has also been used by AMH minimalists to argue that the emotionally fragile women having abortions would most likely face as many or more mental health problems if they were denied abortion. 245 But again, this argument is based entirely on conjecture. While only a few studies have examined the mental health of women denied abortions, none have found any significant mental health benefits compared to other groups of women. 76 , 188
Still another AMH minimalist argument is that women with prior mental illness may instinctively know they are less likely to cope well with an unwanted pregnancy, so the higher rate of abortion among women with mental illness is actually a sign of these women choosing abortion wisely. 106 , 107 Again, this is entirely speculation. It ignores the likelihood that mentally ill women, especially those with a history of being abused, may simply be more susceptible to being pressured into unwanted abortions 45 like Allie All-Risks. Moreover, it ignores the ethical obligation of caregivers to discourage, rather than enable, patterns of behavior that may be self-destructive.
Rather than just assume that mentally ill women are wisely inspired to choose abortion more often than mentally healthy women, would it not be best to screen women seeking abortions for mental illness so women can be counseled in a manner that more fully addresses their needs in the context of their mental illness? 25 , 36 As previously noted, while abortion may relieve some stresses, it may also create new ones.
Moreover, bearing children may actually contribute to mental health improvements through direct biological effect, 150 , 205 , 206 by expanding and strengthening interpersonal relationships with the child(ren) and others, 151 , 152 , 154 , 207 or by behavioral adaptations that may replace risk-taking with self-improving behaviors. These benefits may also apply to bearing unplanned children. Indeed, given how common unplanned pregnancies are throughout the millennia, it could be argued that female biology has evolved mechanisms in order to adapt and adjust to unexpected pregnancies.
In short, the argument that higher rates of mental illness following abortion are simply due to mentally ill women being wise enough to choose abortion more often is simply not supported by any statistically validated research. Instead, the opposite argument, that giving birth is more likely to produce mental health benefits, is more plausible and better supported by actual data.
It should also be noted that while we are aware of only one record linkage study examining mental health effects for women without any history of mental health issues , that study (by AMH minimalists) revealed that a history of abortion was associated with a significantly increased risk (risk ratio (RR) = 1.18; 95% CI = 1.03–1.37) of postpartum depression after a first live birth. 80
Closely related to the pre-existing mental illness issue is the finding that women with a history of abortion also have higher rates of abuse and violence in their lives. According to this argument, violence 106 , 110 or childhood adversities, 106 not abortion, are the most likely cause of higher rates of mental illness among women with a history of abortion. This hypothesis is contradicted, however, by studies which have shown that there are higher rates of mental illness associated with abortion even after controlling for violence. 94 , 109 More importantly, it is a mistake to engage in either/or arguments; a both/and approach is both more likely and more productive. Clearly, a history of abuse contributes to a heightened risk of both pregnancy and abortion, especially abortions to satisfy the demands of others. At the same time, clinical experience reveals that issues related to abuse and abortion can become deeply entangled. Efforts to treat based on an either/or attribution are most likely to be frustrated. Progress is most likely to be made when both the abuse and abortion experiences are holistically addressed. 45
While it important to study the interactions between exposure to violence and abortion on mental health, it is also important to consider that there may be two-way interactions. Surveys of women entering into post-abortion counseling reveal high percentages reporting elevated feelings of anger (81%), rage (52%), more easily lost temper (59%), and more violent behavior when angered (47%) following their abortions, which can obviously increase incidence rates of subsequent intimate partner violence. 45 Moreover, in the same sample, in which 56% reported suicidal feelings and 28% reported attempting suicide (with over half trying more than once), there are case studies of women “pushing the buttons” of a violent partner because they believed they did not “deserve to live.” 45 This escalation of violence following abortion may help to explain the elevated rate of homicide among women with a history of abortion. 88 , 232 , 246 For these reasons, given the multiple pathways for interactions between abortion and violence, studies that fail to distinguish between violence before and following abortion are methodologically flawed. 110 , 247
While prior abuse and mental health problems receive the most blame for why women with a history of abortion have higher rates of mental illness, a few AMH minimalists insist that the blame for mental illness following abortion can always be shifted to other risk factors. 248 For example, when Steinberg et al. 30 found that substance abuse rates were significantly associated with abortion even after controlling for dozens of other risk factors, they dismissed their own findings with the assertion that these effects are most likely due to as yet unidentified common risk factors.
In response, AMH proponents argue that (a) the burden of proving safety and effectiveness is on the proponents of a medical treatment and (b) given the weight of the evidence, it is far more logical to accept that abortion is at least a contributing factor that may work in concert with any number of other contributing factors.
In addition, denying that abortion directly contributes to mental health problems is illogical given the fact that so many of the risk factors identified by AMH minimalists themselves (see Table 1 ) are specifically part of the abortion experience. These include feeling pressured to abort by others; negative moral views of abortion; low expectation of coping well after an abortion; ambivalence about the abortion decision; and feelings of attachment or commitment to a pregnancy that is meaningful or wanted. 25 , 35 , 249
In other words, given what we know of the risk factors associated with mental illness after abortion, many of them are directly enmeshed in the abortion experience; they are not fully independent of the pregnancy and abortion experience. Therefore, even to the degree that mental illnesses can be associated with common risk factors for both unintended pregnancy and abortion, such as a history of sexual abuse, the intermeshing of elevated risk for pregnancy, abortion, and mental health issues precludes the conclusion that abortion does not contribute in any way to the observed problems. The only support for that argument comes from ideology, not from any statistically validated studies. For example, an incest victim may be at greater risk of a high school pregnancy with the first boyfriend that she imagines will be able to free her from an abusive step-father. 250 She may also be at greater risk to being pressured into an unwanted abortion. While it would be a mistake to blame the abortion for all of her subsequent mental health problems, even if a subsequent suicide note focuses on the abortion, it is ludicrous to assert that her abortion did not contribute to her problems. Moreover, it is also evident that the failure of healthcare providers to identify the risk factors that made her a poor candidate for abortion missed an opportunity to assist her in using her pregnancy to break a cycle of exploitation and trauma.
Finally, it should be noted that AMH minimalists frequently cite studies showing that women who deliver an unintended pregnancy have more subsequent problems than women who only have intended pregnancies. 248 From this base of evidence, they argue that since women who deliver unintended pregnancies have more problems, with mental health and otherwise, it follows that access to abortion helps to reduce the problems associated with unintended pregnancies. But this argument falsely presumes that abortion puts women who have unintended pregnancies back into the category of women who have never had an unintended pregnancy, and that all intended pregnancies are carried to term. But there are not just two groups: (a) women with “perfect” reproductive lives and (b) women with a history of unintended pregnancies. There is a third group, (c) women who have had abortions, who may fare worse than either of the other two groups.
While AMH proponents do not dispute that on average women with unintended pregnancies may face more problems than women who have perfect reproductive lives, it appears likely that they still have fewer problems than women who abort. Indeed, as previously discussed, not a single study has found evidence that the mental health of women who deliver an unintended pregnancy is worse than that of women who have abortions. 69 , 72 , 75 , 76 , 86 , 90 , 92 , 98 , 188 To the contrary, the only statistically significant findings indicate that women who abort are likely to have more mental health problems than those who deliver their unintended pregnancies. 17
The controversy over abortion related PTSD is more political than scientific
AMH minimalists often reserve the greatest scorn for statements made by AMH proponents that abortion can be a traumatic experience that may contribute to PTSD. 4 , 251 , 252 But this opposition seems to be driven more by a desire to silence abortion skeptics than to honestly report on the connections between abortion and traumatic reactions as revealed in the literature.
First, it is notable that all pregnancy outcomes are associated with some PTSD risk. Both vaginal and cesarean deliveries can be experienced as traumatic with a corresponding risk of PTSD. 225 , 253 – 255 Miscarriage and other natural pregnancy losses are also consistently associated with increased risk of PTSD. 170 , 222 , 256 – 258 It should therefore come as no surprise that induced abortion is also consistently found to be associated with the onset of PTSD symptoms. 21 , 39 , 50 , 60 , 170 , 225 , 259 – 269 Notably, a history of induced abortion is also a risk factor for the onset of PTSD following subsequent pregnancy outcomes, 170 , 225 , 260 , 270 so the effects of abortion may not always be immediate but may be triggered by subsequent deliveries or natural losses, or even subsequent non-pregnancy-related events. 271 These findings are consistent with the insight that multiple traumas and related life experiences may contribute to the triggering of PTSD symptoms.
Given the weight of the many statistically validated studies cited above, much less than the reports of clinicians and women who attribute PTSD symptoms to their abortions, it seems evident that the effort of a few AMH minimalists to categorically deny that abortion can contribute to traumatic reactions is driven by ideological considerations, not science. That said, it should also be noted that not all women will experience abortion as traumatic. Moreover, the susceptibility of individuals to experience PTSD symptoms can also vary based on many other pre-existing factors, including biological differences. So the risk of individual women will vary, as it does for every type of psychological reaction. Still, when even the chair of the APA’s TFMHA has reported identifying abortion-specific cases of PTSD in one of her own studies, 39 the claim that abortion trauma is a “myth” advanced purely for the purposes of anti-abortion propaganda it itself nothing more than pro-abortion propaganda. 252
The evidence is clear that some women do experience abortion as a trauma. The prevalence rates and pre-existing risk factors may continue to be disputed, but the fact that abortion contributes to PTSD symptoms in at least a small number of women is a settled issue.
Recommendations for research and collaboration
Good research is essential for both healthcare providers and patients. Better information about the risks and benefits associated with abortion should contribute to better screening, better risk–benefit assessments, and better disclosures to patients, 23 that will help to shape the expectations of patients and those who advise them. Better information will also improve the identification of at risk patients who may benefit from referrals to post-abortion counseling.
As previously discussed, while the ideological divides between AMH minimalists and proponents will continue to shape how each side interprets the data, these differing viewpoints actually provide an opportunity for improving the collection of useful data, analyses of the available data, and more thorough interpretations of research findings. Therefore, healthcare providers and patients would be better served by AMH minimalists and AMH proponents both bringing their various perspectives to bear on research efforts in a more cooperative fashion.
Whenever possible, research teams should include both AMH minimalists and AMH proponents. Such cooperation would improve methodologies by better addressing the differing concerns of each perspective at the time of the study design. Collaboration in the writing of introductions and conclusions to such studies would also be improved by bringing balance to both perspectives and by reducing the tendency to overgeneralize results of specific analyses.
More specific opportunities for collaboration and better research are discussed below.
Expanding the research goals
A major problem with abortion research and reviews is a failure to address all of the relevant questions which need to be asked, investigated, and answered. For example, the team from the National Collaborating Center for Mental Health (NCCMH) that wrote a review of AMH issues for the Academy of Medical Royal Colleges in 2011 strictly limited their investigation to only three questions: “(1) How prevalent are mental health problems in women who have an induced abortion? (2) What factors are associated with poor mental health outcomes following an induced abortion? (3) Are mental health problems more common in women who have an induced abortion when compared with women who deliver an unwanted pregnancy?” 5 Most notably, the NCCMH team chose to ignore the question specifically posed for it to investigate in the 2008 Royal College of Psychiatrists position statement on abortion, namely, “whether there is evidence for psychiatric indications for abortion” 272 (emphasis added). Given the lack of any evidence for psychiatric indications for abortion, it seems likely that the NCCMH decided to ignore this question because it echoed previous allegations that UK law was not being followed in regard to limiting abortion to cases where there are therapeutic benefits. 273
Many additional questions were raised during the consultation process when the NCCMH team invited comments and suggestions from experts. But all of these questions were summarily rejected by the NCCMH team as being “beyond the scope” of their review, even though they acknowledged that many of these other questions were equally important to the three questions they had chosen. 274 Indeed, a reading of the consultation report, which was effectively the peer review given to the paper, reveals general dissatisfaction with the three questions chosen by the NCCMH team and with many of their choices in methodology and overstatement or understatement in their conclusions. The consultation report anticipated the many criticisms of the final report 19 , 275 and revealed that NCCMH team was not very responsive to the issues and concerns raised during this peer review. Arguably, the NCCMH team’s unstated mission was to protect the status quo, and so they limited themselves to questions and methodological choices that would allow them to achieve that predetermined goal.
The following is a list of some key research questions that should be addressed in future studies and reviews. It was developed, in part, by using the NCCMH consultation report as a starting point: 274
How prevalent are mental health problems in women who carry unplanned pregnancies to term compared to women who deliver wanted pregnancies, to women who have no children, and to women who have abortions?
Given that women may experience a range of reactions in the near term and over a period of many years, what are the cumulative rates of negative reactions over a long period of time (including a minimum of 30 years) and what are the temporal, cross-sectional prevalence rates relative to various risk factors that may contribute to these temporal differences?
Among women who do experience negative emotional reactions (not limited to mental illness) which they attribute to their abortions, what reactions are reported?
What treatments are most effective?
What statistically validated indicators predict when the mental health risks of continuing a pregnancy are greater than if the pregnancies were aborted?
What statistically validated risk factors predict negative outcomes following one abortion, two abortions, and three or more abortions compared to each available comparison group?
What factors, if any, are associated with improved mental health following abortion compared to similar women who carry a similarly problematic pregnancy to term?
Among women with pre-existing mental health issues, what factors predict a likelihood that abortion may contribute to a reduction in mental health problems (intensity, duration, and number of mental health issues), and what factors predict a likelihood that abortion may contribute to an increase in mental health problems?
Among women without pre-existing mental health issues, what factors predict a likelihood that abortion may protect good mental health, and what factors predict a likelihood that abortion may contribute to subsequent mental health problems?
Is presenting for an abortion, or a history of abortion, a meaningful diagnostic marker for higher rates of mental illness and related problems that can be timely addressed by appropriate offers of care?
In evaluating the risk–benefits profile of a specific patient, what criteria should be met in order to reach an evidence-based conclusion that the benefits of abortion are most likely to exceed the risks?
In cases of pregnancy following rape or incest, what are the short- and long-term mental health effects associated with each of the following outcomes: (a) abortion, (b) miscarriage or stillbirth, (c) childbirth and adoption, and (d) childbirth and raising the child?
Is abortion associated with an increase in rapid repeat pregnancies, that is, “replacement pregnancies?” If so, what portion are delivered, aborted, or miscarried?
Does a history of abortion contribute to the strengthening or weakening of the woman’s relationships with her partner and/or others?
What are the mental health effects of the abortion experience, if any, on men?
What are the mental health and developmental effects of the abortion experience, if any, on previously born children and/or subsequently born children?
Does a history of abortion contribute to or hinder bonding and parenting of previous and/or subsequently born children?
National prospective longitudinal studies specific to reproductive and mental health
While a number of analyses have been published based on longitudinal studies, none of these studies were designed to specifically investigate the intersection between AMH issues. The need for better longitudinal studies to investigate AMH has been recognized in other major reviews, 4 , 24 , 274 yet the call for such research has not yet been heeded.
We recommend that the value of such longitudinal studies would be vastly increased by expanding the goal of data collection to encompass not just mental health effects associated with abortion but also with all reproductive health issues from first menses to menopause. This would assist in research related to infertility, miscarriage, assisted reproductive technologies, postpartum reactions, premenstrual syndrome, and more. And given the interactions with multiple pregnancy outcomes already seen in AMH research, 88 , 94 , 170 , 203 comprehensive reproductive health histories are needed in any case.
Most importantly, the design and management of such studies should include both AMH minimalists and AMH proponents. An explicit objective should be ensuring that every line of questioning either side considers important is included. When both sides contribute to the design of such studies and have equal access to the same data, concerns about suppressed findings or incomplete analyses will be dramatically reduced … at least after re-analyses. When both sides have equal access to better data, it is more likely that the areas of consensus will increase.
The value of longitudinal studies would also be enhanced by seeking the consent of participants to link their medical records to their questionnaires. This would be most helpful given the fact that many women are reluctant to reveal abortion information even in responding to a confidential questionnaire. Since women’s willingness to share data may vary over time, this request for record linkage should perhaps be offered multiple times over the course of the longitudinal study. While many will likely refuse this option, the refusal to permit record linkage is itself a data point for analyzing patterns associated with concealment and dropout. Along the same lines, at each wave there should be included a query regarding the level of stress associated with completing the questionnaire. 183 This may also help to better understand and estimate the effects of women subsequently dropping out.
Finally, it should be noted that it has already been shown that there may be significant differences in women’s experiences relative to different cultures and nationalites. 50 Therefore, it is highly recommended that longitudinal studies to comprehensively investigate the intersections between mental and reproductive health should be funded in multiple countries.
Data sharing for re-analyses should be rule rather than the exception
It is precisely because data can be selectively analyzed and interpreted to produce slanted results, 131 – 133 that data should be made available for re-analyses by third parties. 276 Data sharing also reduces the costs of research and magnifies the contribution volunteers make to science by making their non-identifying information accessible to more scientists, which presumably most volunteers would prefer as their participation is generally intended to help science in general, not specific research teams. Most importantly, data sharing enhances confidence in the reliability of research findings, especially when related to controversial issues. Unfortunately, though many publications and professional organizations encourage or require post-publication sharing of data, in practice many researchers across many disciplines evade data sharing. 277
Support for data sharing, at least in theory, is found in the APA’s ethics rule 8.14, which states that following publication of their results, research psychologists should share the data for reanalysis by others. 278 But this principle has been frequently ignored, 279 – 281 especially in regard to abortion research. For example, the chair of the APA’s own TFMHA, Brenda Major, has repeatedly refused to allow data she collected on abortion patients to be subject to reanalysis by AMH proponents. She even refused to comply with a request for the data from the US Department of Health and Human Services, even though the study was funded by that agency. 140
Such data hoarding undermines confidence not only in the published findings of a specific study but also diminishes the value of syntheses or reviews relying on those unverified findings.
Data sharing is especially important when the process of collecting data may be blocked by ideological litmus tests. For example, abortion providers are naturally unlikely to cooperate with studies initiated by AMH proponents who they perceive as opponents of their work. On the contrary, they have frequently cooperated with AMH minimalists—precisely because of their shared ideology. Implicit in granting that cooperation may be the expectation that pro-choice researchers will not report any findings that may contribute to anti-abortion rhetoric. Conversely, many post-abortion counseling programs may also limit their cooperation to AMH proponents whom they perceive as most accepting and supportive of the issues raised by their clientele. 88
In both cases, the ideological alignments required to collect data may create biases in the design, analysis, and reporting of results. This does not mean that meaningful results cannot be obtained. But it does mean that such results should always be presumed to reflect sample and investigator biases until the findings have been confirmed in reanalyses conducted by investigators of all perspectives. It is only through equal access to the data that consensus will grow around results which survive reanalyses. It is also through this process that new research objectives will be better identified in response to these reanalyses.
Responsiveness to requests for additional analyses
In many cases, legal restrictions (government or contractual) may bar the sharing of underlying data. In such cases, reasonable requests for additional information, tables, and reanalyses should be honored through personal communication, publication of a response, or, if a major reanalysis is required, in publication of a subsequent paper. Such cooperation is especially important in regard to data sets that have access restrictions, such as those collected by government agencies.
For example, the centralized medical records of Denmark have provided some of the best record linkage studies in the world. However, when it comes to mental health effects associated with abortion, there is strong evidence that significant findings are being suppressed for ideological reasons. The arguments and evidence for this assertion are given below.
In 2011, Munk-Olsen et al. 82 published an analysis of Danish medical records to investigate first time psychiatric contact in the first year following a first abortion or first delivery. The analyses revealed that women who aborted had double the risk of psychiatric contact (OR = 2.18). But this finding was discounted by the finding that aborting women also had higher rates of outpatient psychiatric contact in the 9 months prior to their abortions (including the time they were pregnant) compared to the 9 months prior to a live birth. Munk-Olsen later conceded that this mixture of pre-conception time and pregnancy time created a baseline that “may not be directly compatible.” 227 But this was just one of many major weaknesses in the design and reporting of this highly criticized study. 282
Another methodological problem was the decision to include women who had one or more abortions prior to their first delivery into the delivery group. This decision is especially problematic since a history of abortion is significantly associated with higher rates of mental illness during and after subsequent pregnancies. 78 , 80 , 99 , 170 , 197 , 217 Notably, when Munk-Olsen was asked to provide a simple count of the number of women in her analyses who had both abortions and deliveries and the percentage of those who had psychiatric contact, she refused this and all other requests for more details. 227
Before examining the inconsistencies revealed in subsequent Munk-Olsen et al. 82 studies, it is relevant to compare her abortion study to three very similar record linkage studies conducted by AMH proponents conducted a decade earlier. These prior studies examined the differences between abortion and delivery in regard to inpatient psychiatric treatments, 89 outpatient psychiatric treatments, 97 and sleep disorders. 87 The designs of those studies were superior to Munk-Olsen’s in several respects: (a) in each case, controls for prior psychiatric inpatient treatment were employed for a longer period of time, a 12- to 18-month period prior to the estimated date of conception for each woman; (b) there was complete segregation of women relative to exposure to abortion; (c) mental health outcomes were reported showing variations relative to different age groups; and (d) results were shown over multiple time periods: 0–90 days, 0–180 days, first year, second year, third year, fourth year, and 0–4 years.
Normally, one would expect Munk-Olsen to have at least replicated, if not improved on, the methodology employed in these prior record linkage studies. Instead, the methodological choices she made severely narrowed the range of her investigation. Studies that are narrowly drawn can only support narrow conclusions. This is especially true since Munk-Olsen also excluded any analyses of the effects of multiple abortions, which are known to be associated with even higher rates of negative reactions 94 , 112 and also make up the majority of all abortions being performed. 64
Concerns about selective reporting are heighted by the fact that Munk-Olsen subsequently published numerous studies on mental health associated with childbirth in which, once again, she refused requests to supply data for findings associated with abortion. For example, using the same data set, Munk-Olsen published findings that reported
Psychiatric treatment following delivery was associated with a fourfold increased risk of a diagnosis of bipolar disorders within the next 15 years; 283
Rates of antidepressant use and mental health treatments 12 months prior to childbirth and 12 months after; 208
Elevated rates of psychiatric disorders following miscarriage or stillbirth; 217
Rates of postpartum depression following delivery of IVF pregnancies; 284
Rates of primary care treatments before, during, and after pregnancies in which women experienced postpartum psychiatric episodes; 210
Average monthly rates of psychological treatment and prescriptions before and after childbirth. 209
In each of these cases, her analyses and conclusions were flawed by the failure to address the effects of prior fetal loss, which are known to increase the risk of psychiatric disorders during and after subsequent pregnancies. 78 , 170 , 212 , 225 , 285 , 286
While in most cases she simply omitted abortion history from her analyses, 208 – 210 , 283 in two cases she used abortion history as a control variable 217 , 284 but omitted any statistics showing how this control affected the results. Clearly, the only reason to use abortion history as a control is if it has a significant independent effect on mental health outcomes.
The possibility that Munk-Olsen simply overlooked these opportunities to report on effects associated with abortion is disproven by the fact that in each case Munk-Olsen rejected both published 141 , 227 and unpublished requests for details relative to the effects of abortion on the outcomes studied. Even a request for a simple count of the number of women exposed to abortion in each of Munk-Olsen’s comparison groups was refused. 141
All of the above factors give credence to the concern that there is a selective withholding of results, by Munk-Olsen and other AMH minimalists. Moreover, given the evidence that abortion and miscarriage impacts mental health during subsequent pregnancies, 78 , 80 , 99 , 170 , 197 , 203 , 212 – 221 it is clear that every study examining the intersection between mental and reproductive health may be misleading if it fails to include analyses associated with pregnancy loss. Without such analyses, effects associated with pregnancy loss may be wrongly attributed to childbirth.
For example, there is strong evidence from both record linkage 89 , 97 and case-matched studies 287 that a history of abortion is associated with a threefold increase in bipolar disorder. Therefore, Munk-Olsen et al.’s 283 decision to exclude analyses related to fetal loss from her study of bipolar disorders following postpartum depression severely undermines her conclusion that this negative outcome is due to childbirth alone precisely because she chose to ignore, or at least not publish, findings associated with fetal loss.
The combination of Munk-Olsen’s failure to publish these results without being asked, combined with her refusal to respond to requests for reanalysis, 141 , 227 strongly suggests a pattern of selective reporting and obfuscation. If the additional analyses requested actually supported her previous assertion that prior mental health fully explains the higher rates of mental illness seen among women who have aborted 82 , 107 it seems clear that she should be rushing to publish these requested analyses precisely to silence skeptics.
In short, whenever either AMH minimalists or AMH proponents refuse to respond to queries for reanalyses of published findings, they are increasing distrust and weakening the credibility of all conclusions based on their previously published research. This creates real obstacles in the advance of evidence-based medicine, informed consent practices, and ultimately in the medical care of women. The advance of scientific investigations into reproductive mental health can only be enhanced by generously responding to requests for details and re-analyses that clarify the interpretation of published findings.
Recommendations for editors and peer reviewers
As previously discussed, there is strong evidence that individual biases may unfairly bias editors and reviewers against findings that challenge their preconceived notions. 118 – 123 Biases against “conservative” viewpoints, which may attach to the AMH controversy, are especially common. 125 – 128 , 130
Editors should guard against this bias by seeking a mix of peer reviewers, including both AMH minimalists and AMH proponents. For reasons discussed previously, while recognizing that every study in this area will have methodological weaknesses and that no sample can be perfect, editors should be blind to the results and focus their evaluation of peer review comments on the appropriateness and adequacy of the methodology and study sample. Editors should be alert to criticisms that appear to reflect a reviewer’s bias against results which support an undesired conclusion, especially when the methodology employed is comparable to studies that would be accepted for publication in any other field of research.
A good test of bias is to simply imagine that the results were flipped, 123 with the ORs showing benefits to abortion compared to delivering an unwanted pregnancy, for example. If the reviewer’s or editors reactions to the paper would most likely have been in the opposite direction, that reaction is obviously driven by a bias for preferred results.
Editors and peer reviewers should also strive to ensure that all studies relating to the intersection of mental and reproductive health include, whenever possible, analyses that delineate findings relative to exposure to all prior pregnancy outcomes, including both natural pregnancy losses and induced abortions. 141 , 227 This is important for several reasons. First, there is consensus even among AMH minimalists that better data are needed on the effects of pregnancy loss on mental health. 4 , 274 Second, there is clear and convincing evidence that exposure to pregnancy losses (both natural and induced) may have a significant impact on women’s health during and after subsequent pregnancies and at other times in women’s lives. 80 , 88 , 94 , 99 , 112 , 170 , 212 , 285
When data on abortion and miscarriage history are available, but not included in published findings, this raises concerns about concealment of findings that the authors may be afraid will bolster the position of their ideological rivals. 141 , 227 Alert reviewers and editors should routinely ask researchers to include in their tables of results analyses relevant to the number of exposures to abortion and natural pregnancy losses. Without such requests (a) the literature will continue to be deprived of meaningful data and (b) selective reporting may falsely attribute negative mental health issues to childbirth.
Limitations
The purpose of this review of the medical literature on AMH was to examine the areas of agreement and disagreement, the reasons for disagreement, and the opportunities for improved research and collaboration. The method I used began with a review of reviews published since 2005 4 – 10 , 12 – 19 , 21 , 22 and an examination of the studies cited in these reviews.
Given the difficulties previously discussed in conducting any conclusive studies, the breadth of issues examined in this review, and the range of theories and opinions of the authors of the reviews and studies examined, it is out of the scope of this, or any, review to fully address every view or concern. With that limitation in mind, however, this review does catalog a broader range of relevant issues than any previous reviews. In doing so, this review does not offer the last word on the AMH controversy. Instead, it seeks to expand and continue the conversation, inviting more detailed responses, criticism, and elaboration regarding the issues identified herein.
While there will continue to be differences of opinion between AMH minimalists and AMH proponents, there is sufficient common ground upon which to build future efforts to improve research and meaningful re-analyses. Common ground exists regarding the very basic fact that at least some women do have significant mental health issues that are caused, triggered, aggravated, or complicated by their abortion experience. In many cases, this may be due to feeling pressured into an abortion or choosing an abortion without sufficient attention to maternal desires or moral beliefs that may make it difficult to reconcile one’s choice with one’s self-identity.
There is also common ground regarding the fact that risk factors identifying women who are at greater risk, including a history of prior mental illness, can be used to identify women who may benefit from more pre-abortion and post-abortion counseling. Additional research regarding risk factors, and indicators identifying when abortion may be most likely to produce the benefits sought by women without negative consequences, can and should be conducted through major longitudinal prospective studies.
Finally, there is common ground on the need for better research. That fact alone is a strong argument for mixed research teams, collaboration in the design of longitudinal studies available for analysis by any researcher (without ideological screenings), data sharing and more responsive cooperation in responding to requests for reanalysis. All of these steps will help to provide healthcare workers with more accurate information for screening, risk–benefits assessments, and for offering better care and information to women both before and after abortion and other reproductive events.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: D.C.R.’s efforts were funded as part of his regular duties as Director of Research with the Elliot Institute.

- 1. Wilmoth GH. Abortion, public health policy, and informed consent legislation. J Soc Issues 1992; 48(3): 1–17. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Painter J, Ashe T. Cross-national comparison of the presence of climate scepticism in the print media in six countries, 2007–10. Environ Res Lett 2012; 7(4): 044005. [ Google Scholar ]
- 3. MacNair RM. Introduction: understanding perspectives. In: MacNair RM. (ed.) Peace psychology perspectives on abortion. Kansas City, MO: Feminism & Nonviolence Studies Association, 2016, p. 316. [ Google Scholar ]
- 4. Major B, Appelbaum M, Beckman L, et al. Report of the APA Task Force on mental health and abortion. Washington, DC: American Psychological Association, 2008, 105 pp, http://www.apa.org/pi/women/programs/abortion/mental-health.pdf [ Google Scholar ]
- 5. National Collaborating Centre for Mental Health. Induced abortion and mental health: a systematic review of the mental health outcomes of induced abortion, including their prevalence and associated factors. London: Academy of Medical Royal Colleges, 2011, http://www.aomrc.org.uk/wp-content/uploads/2016/05/Induced_Abortion_Mental_Health_1211.pdf [ Google Scholar ]
- 6. Charles VE, Polis CB, Sridhara SK, et al. Abortion and long-term mental health outcomes: a systematic review of the evidence. Contraception 2008; 78: 436–450. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Major B, Appelbaum M, Beckman L, et al. Abortion and mental health: evaluating the evidence. Am Psychol 2009; 64(9): 863–890. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Steinberg JR. Later abortions and mental health: psychological experiences of women having later abortions—a critical review of research. Womens Health Issues 2011; 21(3): S44–S48. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Hall M, Chappell LC, Parnell BL, et al. Associations between intimate partner violence and termination of pregnancy: a systematic review and meta-analysis. PLoS Med 2014; 11(1): e1001581. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Horvath S, Schreiber CA. Unintended pregnancy, induced abortion, and mental health. Curr Psychiatry Rep 2017; 19(11): 77. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Thorp JM, Hartmann KE, Shadigian E. Long-term physical and psychological health consequences of induced abortion: review of the evidence. Obstet Gynecol Surv 2003; 58(1): 67–79. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Casey P, Oates M, Jones I, et al. Invited commentaries on… Abortion and mental health disorders. Br J Psychiatry 2008; 193(6): 452–454. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Coleman PK. Induced abortion and increased risk of substance abuse: a review of the evidence. Curr Womens Health Rev 2005; 1(1): 21–34 [ Google Scholar ]
- 14. Coleman PK, Reardon DC, Strahan T, et al. The psychology of abortion: a review and suggestions for future research. Psychol Health 2005; 20: 237–271. [ Google Scholar ]
- 15. Coleman PK. Abortion and mental health: quantitative synthesis and analysis of research published 1995-2009. Br J Psychiatry 2011; 199: 180–186. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Bellieni CV, Buonocore G. Abortion and subsequent mental health: review of the literature. Psychiatry Clin Neurosci 2013; 67(5): 301–310. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Fergusson DM, Horwood LJ, Boden JM. Does abortion reduce the mental health risks of unwanted or unintended pregnancy? A re-appraisal of the evidence. Aust N Z J Psychiatry 2013; 47(9): 819–827. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Gurpegui M, Jurado D. Psychiatric complications of abortion. Cuad Bioét 2009; 20(70): 381–392. [ PubMed ] [ Google Scholar ]
- 19. Ney PG. A common sense scientific critique of the NCCMH and Royal College of Psychiatry Review. Webmed Cent 2013; 4(10): 1–13. [ Google Scholar ]
- 20. Turk AM. How we got there from here: transforming the debate over abortion. In: MacNair RM. (ed.) Peace psychology perspectives on abortion. Kansas City, MO: Feminism & Nonviolence Studies Association, 2016, p. 312. [ Google Scholar ]
- 21. Daugirdaitė V, van den Akker O, Purewal S. Posttraumatic stress and posttraumatic stress disorder after termination of pregnancy and reproductive loss: a systematic review. J Pregnancy 2015; 2015: 646345 (14 pp.). [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Hanschmidt F, Linde K, Hilbert A, et al. Abortion stigma: a systematic review. Perspect Sex Reprod Health 2016; 48(4): 169–177. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Coleman PK, Reardon DC, Lee MB. Women’s preferences for information and complication seriousness ratings related to elective medical procedures. J Med Ethics 2006; 32(8): 435–438. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Major B, Cozzarelli C. Psychosocial predictors of adjustment to abortion. J Soc Issues 1992; 48(3): 121–142. [ Google Scholar ]
- 25. Reardon DC. Abortion decisions and the duty to screen: clinical, ethical, and legal implications of predictive risk factors of post-abortion maladjustment. J Contemp Health Law Policy 2003; 20(1): 33–114. [ PubMed ] [ Google Scholar ]
- 26. Royal College of Psychiatrists. Position statement of women’s mental health in relation to induced abortion. London, 2008, https://www.wthrockmorton.com/2008/08/20/royal-college-of-psychiatrists-statement-on-abortion-and-mental-health/ [ Google Scholar ]
- 27. Shuping M. Wantedness & coercion: key factors in understanding women’s mental health after abortion. Assoc Interdiscip Res Values Soc Chang Res Bull 2011; 23(2): 8. [ Google Scholar ]
- 28. Shusterman L. The psychosocial factors of the abortion experience: a critical review. Psychol Women Q 1976; 1: 79–106. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Shusterman L. Predicting the psychological consequences of abortion. Soc Sci Med Med Psychol Med Sociol 1979; 13: 683–689. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Steinberg JR, McCulloch CE, Adler NE. Abortion and mental health: findings from the national comorbidity survey-replication. Obstet Gynecol 2014; 123(2 Pt 1): 263–270. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Lehmann C. Psychiatrists can play critical role in pregnancy decisions. Psychiatr News 2003; 38(13): 8–43. [ Google Scholar ]
- 32. Athanasiou R, Oppel W, Michelson L, et al. Psychiatric sequelae to term birth and induced early and late abortion: a longitudinal study. Fam Plann Perspect 1973; 5(4): 227–231. [ PubMed ] [ Google Scholar ]
- 33. Belsey EM, Greer HS, Lal S, et al. Predictive factors in emotional response to abortion: King’s termination study —IV. Soc Sci Med 1977; 11(2): 71–82. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Casey PR. Abortion among young women and subsequent life outcomes. Best Pract Res Cl Ob 2010; 24(4): 491–502. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Coleman PK. Women at risk for post-abortion mental health problems and abortion associated relationship challenges. Post-abortion trauma: possible psychological and existential aftermaths. Rome: Pontifical Academy for Life, 2014, pp. 147–210, http://www.academiavita.org/_pdf/documents/pav/post_abortion_trauma.pdf [ Google Scholar ]
- 36. Lask B. Short term psychiatric sequelae to therapeutic termination of pregnancy. Br J Psychiatry 1975; 126(2): 173–177. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Lemkau J. Emotional sequelae of abortion: implications for clinical practice. Psychol Women Q 1988; 12: 461–472. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Miller W. An empirical study of the psychological antecedents and consequences of induced abortion. J Soc Issues 1992; 48(3): 67–93. [ Google Scholar ]
- 39. Major B, Cozzarelli C, Cooper ML, et al. Psychological responses of women after first-trimester abortion. Arch Gen Psychiatry 2000; 57(8): 777–784. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Stotland NL. Abortion: social context, psychodynamic implications. Am J Psychiatry 1998; 155(7): 964–967. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Torre-Bueno A. Peace after abortion. San Diego, CA: Pimpernel Press, 1997. [ Google Scholar ]
- 42. Johnson TM. Bringing abortion aftercare into the 21st century. Counseling Today, 2013, http://ct.counseling.org/2013/01/bringing-abortion-aftercare-into-the-21st-century/
- 43. De Puy C, Dovitch D. The healing choice: your guide to emotional recovery after an abortion. New York: Simon & Schuster, 1997. [ Google Scholar ]
- 44. Goldstein D. The abortion counseling conundrum. The American Prospect, 2008, http://prospect.org/article/abortion-counseling-conundrum
- 45. Burke T, Reardon DC. Forbidden grief: the unspoken pain of abortion. Springfield, IL: Acorn Books, 2007, 334 pp. [ Google Scholar ]
- 46. Layer SD. Postabortion grief: evaluating the possible efficacy of a spiritual group intervention. Res Soc Work Pract 2004; 14(5): 344–350. [ Google Scholar ]
- 47. Ney PG, Wickett AR. Mental health and abortion: review and analysis. Psychiatr J Univ Ott 1989; 14(4): 506–516. [ PubMed ] [ Google Scholar ]
- 48. Zimmerman MK. Passage through abortion: the personal and social reality of women’s experiences. New York: Praeger Publishers, 1977, 238 pp. [ Google Scholar ]
- 49. Sihvo S, Bajos N, Ducot B, et al. Women’s life cycle and abortion decision in unintended pregnancies. J Epidemiol Community Health 2003; 57(8): 601–605. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Rue VM, Coleman PK, Rue JJ, et al. Induced abortion and traumatic stress: a preliminary comparison of American and Russian women. Med Sci Monit 2004; 10(10): SR5–SR16. [ PubMed ] [ Google Scholar ]
- 51. Major B, Mueller P, Hildebrandt K. Attributions, expectations, and coping with abortion. J Pers Soc Psychol 1985; 48(3): 585–599. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Smetana J. Reasoning in the personal and moral domains: adolescent and young adult women’s decision-making regarding abortion. J Appl Dev Psychol 1981; 2: 211–226. [ Google Scholar ]
- 53. Major B, Gramzow RH. Abortion as stigma: cognitive and emotional implications of concealment. J Pers Soc Psychol 1999; 77(4): 735–745. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Cozzarelli C, Major B, Karrasch A. Women’s experiences of and reactions to antiabortion picketing. Basic Appl Soc 2000; 22: 265–275. [ Google Scholar ]
- 55. Major B, Zubek JM, Cooper ML, et al. Mixed messages: implications of social conflict and social support within close relationships for adjustment to a stressful life event. J Pers Soc Psychol 1997; 72(6): 1349–1363. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Major B, Cozzarelli C, Sciacchitano AM, et al. Perceived social support, self-efficacy, and adjustment to abortion. J Pers Soc Psychol 1990; 59(3): 452–463. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Steinberg JR, Finer LB. Examining the association of abortion history and current mental health: a reanalysis of the National Comorbidity Survey using a common-risk-factors model. Soc Sci Med 2011; 72(1): 72–82. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Emmerik A, van Kamphuis J. Prevalence and prediction of re-experiencing and avoidance after elective surgical abortion: a prospective study. Clin Psychol Psychother 2008; 15: 378–385. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Broen AN, Moum T, Bödtker AS, et al. Psychological impact on women of miscarriage versus induced abortion: a 2-year follow-up study. Psychosom Med 2004; 66(2): 265–271. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Van Rooyenm M, Smith S. The prevalence of post-abortion syndrome in patients presenting at Kalafong hospital’s family medicine clinic after having a termination of pregnancy. S Afr Fam Pr 2004; 46(5): 21–24. [ Google Scholar ]
- 61. Husfeldt C, Hansen SK, Lyngberg A, et al. Ambivalence among women applying for abortion. Acta Obstet Gynecol Scand 1995; 74(10): 813–817. [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Kero A, Högberg U, Jacobsson L, et al. Legal abortion: a painful necessity. Soc Sci Med 2001; 53(11): 1481–1490. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Cohan CL, Dunkel-schetter C, Lydon J. Pregnancy decision making: predictors of early stress and adjustment. Psychol Women Q 1993; 17(2): 223–239. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Jones R, Singh S, Finer L, et al. Repeat abortion in the United States. Occasional report no. 29. New York, 2006, http://www.popline.org/node/563305 [ Google Scholar ]
- 65. Pazol K, Creanga AA, Burley KD, et al. ; Centers for Disease Control and Prevention (CDC). Abortion surveillance—United States, 2010. MMWR Surveill Summ 2013; 62(8): 1–44. [ PubMed ] [ Google Scholar ]
- 66. Baker A, Beresford T. Informed consent, patient education and counseling. In: Paul M, Lichtenberg E, Borgatta L, et al. (eds) Management of unintended and abnormal pregnancy: comprehensive abortion care. Chichester: Wiley-Blackwell, 2009, https://books.google.com/books?hl=en&lr=&id=iK7xrRr2p9sC&oi=fnd&pg=PA27&dq=Management+of+Unintended+and+Abnormal+Pregnancy:+Comprehensive+Abortion+Care&ots=S1VJfHUdVD&sig=C5Yqy9-jPROhk2wPikMS87GTWTo#v=onepage&q=ManagementofUnintendedandAbnormalPregna [ Google Scholar ]
- 67. Gissler M, Karalis E, Ulander VM. Decreased suicide rate after induced abortion, after the Current Care Guidelines in Finland 1987–2012. Scand J Public Health 2014; 43(1): 99–101. [ DOI ] [ PubMed ] [ Google Scholar ]
- 68. Upadhyay UD, Cockrill K, Freedman LR. Informing abortion counseling: an examination of evidence-based practices used in emotional care for other stigmatized and sensitive health issues. Patient Educ Couns 2010; 81(3): 415–421. [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Schmiege S, Russo NF. Depression and unwanted first pregnancy: longitudinal cohort study. BMJ 2005; 331(7528): 1303. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Reardon DC. Missed opportunities and overstated results in anxiety and quality of life study following termination of pregnancy. Acta Obstet Gynecol Scand 2016; 96: 382. [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Cougle JR, Reardon DC, Coleman PK. Depression associated with abortion and childbirth: a long-term analysis of the NLSY cohort. Med Sci Monit 2003; 9(4): CR105–CR112. [ PubMed ] [ Google Scholar ]
- 72. Cougle JR, Reardon DC, Coleman PK. Generalized anxiety following unintended pregnancies resolved through childbirth and abortion: a cohort study of the 1995 National Survey of Family Growth. J Anxiety Disord 2005; 19(1): 137–142. [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. David HP. Post-abortion and post-partum psychiatric hospitalization. Ciba Found Symp 1985; 115: 150–164. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Dingle K, Alati R, Clavarino A, et al. Pregnancy loss and psychiatric disorders in young women: an Australian birth cohort study. Br J Psychiatry 2008; 193(6): 455–460. [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Fergusson DM, Horwood LJ, Boden JM. Abortion and mental health disorders: evidence from a 30-year longitudinal study. Br J Psychiatry 2008; 193(6): 444–451. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Gilchrist AC, Hannaford PC, Frank P, et al. Termination of pregnancy and psychiatric morbidity. Br J Psychiatry 1995; 167(2): 243–248. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Gissler M, Hemminki E, Lönnqvist J, et al. Suicides after pregnancy in Finland, 1987-94: register linkage study. BMJ 1996; 313(7070): 1431–1434. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 78. Gong X, Hao J, Tao F, et al. Pregnancy loss and anxiety and depression during subsequent pregnancies: data from the C-ABC study. Eur J Obstet Gynecol Reprod Biol 2013; 166(1): 30–36. [ DOI ] [ PubMed ] [ Google Scholar ]
- 79. Luo M, Jiang X, Wang Y, et al. Association between induced abortion and suicidal ideation among unmarried female migrant workers in three metropolitan cities in China: a cross-sectional study. BMC Public Health 2018; 18(1): 625. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Meltzer-Brody S, Maegbaek ML, Medland SE, et al. Obstetrical, pregnancy and socio-economic predictors for new-onset severe postpartum psychiatric disorders in primiparous women. Psychol Med 2017; 47: 1427–1441. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Morgan CL, Evans M, Peters JR. Suicides after pregnancy. Mental health may deteriorate as a direct effect of induced abortion. BMJ 1997; 314(7084): 902. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 82. Munk-Olsen T, Laursen TM, Pedersen CB, et al. Induced first-trimester abortion and risk of mental disorder. N Engl J Med 2011; 364(4): 332–339. [ DOI ] [ PubMed ] [ Google Scholar ]
- 83. Østbye T, Wenghofer EF, Woodward CA, et al. Health services utilization after induced abortions in Ontario: a comparison between community clinics and hospitals. Am J Med Qual 2001; 16(3): 99–106. [ DOI ] [ PubMed ] [ Google Scholar ]
- 84. Pedersen W. Childbirth, abortion and subsequent substance use in young women: a population-based longitudinal study. Addiction 2007; 102(12): 1971–1978. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Pedersen W. Abortion and depression: a population-based longitudinal study of young women. Scand J Public Health 2008; 36(4): 424–428. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Reardon DC, Cougle JR. Depression and unintended pregnancy in the National Longitudinal Survey of Youth: a cohort study. BMJ 2002; 324(7330): 151–152. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Reardon DC, Coleman PK. Relative treatment rates for sleep disorders and sleep disturbances following abortion and childbirth: a prospective record-based study. Sleep 2006; 29(1): 105–106. [ DOI ] [ PubMed ] [ Google Scholar ]
- 88. Reardon DC, Ney PG, Scheuren F, et al. Deaths associated with pregnancy outcome: a record linkage study of low income women. South Med J 2002; 95(8): 834–841. [ PubMed ] [ Google Scholar ]
- 89. Reardon DC, Cougle JR, Rue VM, et al. Psychiatric admissions of low-income women following abortion and childbirth. CMAJ 2003; 168(10): 1253–1256. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. Reardon DC, Coleman PK, Cougle JR. Substance use associated with unintended pregnancy outcomes in the National Longitudinal Survey of Youth. Am J Drug Alcohol Abuse 2004; 30(2): 369–383. [ DOI ] [ PubMed ] [ Google Scholar ]
- 91. Rees D, Sabia J. The relationship between abortion and depression: new evidence from the fragile families and child wellbeing study. Med Sci Monit 2007; 13(10): CR430–CR436. [ DOI ] [ PubMed ] [ Google Scholar ]
- 92. Steinberg JR, Russo NF. Abortion and anxiety: what’s the relationship? Soc Sci Med 2008; 67(2): 238–252. [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Steinberg JR, Laursen TM, Adler NE, et al. Examining the association of antidepressant prescriptions with first abortion and first childbirth. JAMA Psychiatry 2018; 75: 828–834. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. Sullins DP. Abortion, substance abuse and mental health in early adulthood: thirteen-year longitudinal evidence from the United States. SAGE Open Med 2016; 4: 2050312116665997. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Taft AJ, Watson LF. Depression and termination of pregnancy (induced abortion) in a national cohort of young Australian women: the confounding effect of women’s experience of violence. BMC Public Health 2008; 8: 75. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 96. van Ditzhuijzen J, ten Have M, de Graaf R, et al. Incidence and recurrence of common mental disorders after abortion: results from a prospective cohort study. J Psychiatr Res 2017; 84: 200–206. [ DOI ] [ PubMed ] [ Google Scholar ]
- 97. Coleman PK, Reardon DC, Rue VM, et al. State-funded abortions versus deliveries: a comparison of outpatient mental health claims over 4 years. Am J Orthopsychiatry 2002; 72(1): 141–152. [ DOI ] [ PubMed ] [ Google Scholar ]
- 98. Coleman PKP. Resolution of unwanted pregnancy during adolescence through abortion versus childbirth: individual and family predictors and psychological consequences. J Youth Adolesc 2006; 35(6): 903–911. [ Google Scholar ]
- 99. Coleman PK, Reardon DC, Rue VM, et al. A history of induced abortion in relation to substance abuse during subsequent pregnancies carried to term. Am J Obstet Gynecol 2002; 187(6): 1673–1678. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. Coleman PK, Reardon DC, Cougle JR. Substance use among pregnant women in the context of previous reproductive loss and desire for current pregnancy. Br J Health Psychol 2005; 10(Pt 2): 255–268. [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. Coleman PK, Coyle CT, Shuping M, et al. Corrigendum to “induced abortion and anxiety, mood, and substance abuse disorders: isolating the effects of abortion in the national comorbidity survey” [Journal of Psychiatric Research 2009;43:770–776]. J Psychiatr Res 2011; 45(8): 1133–1134. [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Coleman PK, Maxey CD, Spence M, et al. Predictors and correlates of abortion in the fragile families and well-being study: paternal behavior, substance use, and partner violence. Int J Ment Health Addict 2009; 7(3): 405–422. [ Google Scholar ]
- 103. Mota NP, Burnett M, Sareen J. Associations between abortion, mental disorders, and suicidal behaviour in a nationally representative sample. Can J Psychiatry 2010; 55(4): 239–247. [ DOI ] [ PubMed ] [ Google Scholar ]
- 104. Steinberg JR, Trussell J, Hall KS, et al. Fatal flaws in a recent meta-analysis on abortion and mental health. Contraception 2012; 86(5): 430–437. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 105. Major B. Psychological implications of abortion—highly charged and rife with misleading research. CMAJ 2003; 168(10): 1257–1258. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 106. Steinberg JR, Tschann JM. Childhood adversities and subsequent risk of one or multiple abortions. Soc Sci Med 2013; 81: 53–59. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 107. Munk-Olsen T, Laursen TM, Pedersen CB, et al. First-time first-trimester induced abortion and risk of readmission to a psychiatric hospital in women with a history of treated mental disorder. Arch Gen Psychiatry 2012; 69(2): 159–165. [ DOI ] [ PubMed ] [ Google Scholar ]
- 108. Coyle C. Intimate partner violence. In: MacNair RM. (ed.) Peace psychology perspectives on abortion. Kansas City, MO: Feminism & Nonviolence Studies Association, 2016. [ Google Scholar ]
- 109. Coyle CT, Shuping MW, Speckhard A, et al. The relationship of abortion and violence against women: violence prevention strategies and research needs. Issues Law Med 2015; 30(2): 111–127. [ PubMed ] [ Google Scholar ]
- 110. Russo NF, Denious JE. Violence in the lives of women having abortions: implications for practice and public policy. Prof Psychol Res Pract 2001; 32(2): 142–150. [ Google Scholar ]
- 111. Scott KM, Lim C, Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 2016; 73(2): 150–158. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 112. Coleman PK, Reardon DC, Calhoun BC. Reproductive history patterns and long-term mortality rates: a Danish, population-based record linkage study. Eur J Public Health 2013; 23(4): 569–574. [ DOI ] [ PubMed ] [ Google Scholar ]
- 113. Reardon DC, Coleman PK. Short and long term mortality rates associated with first pregnancy outcome: population register based study for Denmark 1980-2004. Med Sci Monit 2012; 18(9): PH71–PH76. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 114. APA Press Room. APA Task Force finds single abortion not a threat to women’s mental health. American Psychological Association Press Releases, 2008, http://www.apa.org/news/press/releases/2008/08/single-abortion.aspx [ Google Scholar ]
- 115. Jones R, Finer L, Singh S. Characteristics of US abortion patients, 2008. New York: Guttmacher Institute, 2010, http://nyfamilylife.org/wp-content/uploads/2013/11/US-Abortion-Patients.pdf [ Google Scholar ]
- 116. Jones R, Kost K, Singh S, et al. Trends in abortion in the United States. Clin Obstet Gynecol 2009; 52(2): 119–129. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Finer LB Frohwirth LF Dauphinee LA et al.Reasons U.S.. women have abortions: quantitative and qualitative perspectives. Perspect Sex Reprod Health 2005; 37(3): 110–118. [ DOI ] [ PubMed ] [ Google Scholar ]
- 118. Biggs M. The impact of peer review on intellectual freedom. Libr Trends 1990; 39: 145–167. [ Google Scholar ]
- 119. Abramowitz SI, Gomes B, Abramowitz C V. Publish or politic: referee bias in manuscript review. J Appl Soc Psychol 1975; 5(3): 187–200. [ Google Scholar ]
- 120. Armstrong JS. Peer review for journals: evidence on quality control, fairness, and innovation. Sci Eng Ethics 1997; 3(1): 63–84. [ Google Scholar ]
- 121. Peters D, Ceci S. Peer-review practices of psychological journals: the fate of published articles, submitted again. Behav Brain Sci 1982; 5: 187–195. [ Google Scholar ]
- 122. Koehler JJ. The influence of prior beliefs on scientific judgments of evidence quality. Organ Behav Hum Decis Process 1993; 56(1): 28–55. [ Google Scholar ]
- 123. Mahoney MJ. Publication prejudices: an experimental study of confirmatory bias in the peer review system. Cognit Ther Res 1977; 1(2): 161–175. [ Google Scholar ]
- 124. Lord CG, Ross L, Lepper MR. Biased assimilation and attitude polarization: the effects of prior theories on subsequently considered evidence. J Pers Soc Psychol 1979; 37(11): 2098–2109. [ Google Scholar ]
- 125. Goodstein LD, Brazis KL. Psychology of scientist: XXX. Credibility of psychologists: an empirical study. Psychol Rep 1970; 27(3): 835–838. [ Google Scholar ]
- 126. Wright RH, Cummings NA. (eds). Destructive trends in mental health: the well intentioned path to harm. New York, NY: Routledge, 2005, 384 pp. [ Google Scholar ]
- 127. Konnikova M. Is social psychology biased against Republicans? The New Yorker, 2014, http://www.newyorker.com/science/maria-konnikova/social-psychology-biased-republicans
- 128. Duarte JL, Crawford JT, Stern C, et al. Political diversity will improve social psychological science. Behav Brain Sci 2015; 38: e130. [ DOI ] [ PubMed ] [ Google Scholar ]
- 129. Tappin BM, McKay RT. The illusion of moral superiority. Soc Psychol Personal Sci 2017; 8: 623–631. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 130. Inbar Y, Lammers J. Political diversity in social and personality psychology. Perspect Psychol Sci 2012; 7(5): 496–503. [ DOI ] [ PubMed ] [ Google Scholar ]
- 131. Open Science Collaboration. Estimating the reproducibility of psychological science. Science 2015; 349(6251): aac4716. [ DOI ] [ PubMed ] [ Google Scholar ]
- 132. Ioannidis JPA. Why most published research findings are false. PLoS Med 2005; 2(8): e124. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 133. Simmons JP, Nelson LD, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol Sci 2011; 22(11): 1359–1366. [ DOI ] [ PubMed ] [ Google Scholar ]
- 134. Tierney J. Social psychologists detect liberal bias within. The New York Times, 7 February 2011, http://www.nytimes.com/2011/02/08/science/08tier.html?_r=1
- 135. American Psychological Association. Council policy manual: abortion resolutions. American Psychological Association, 1969, p. 1, http://www.apa.org/about/policy/abortion.aspx [ Google Scholar ]
- 136. Coleman PK. Deriving sensible conclusion from the scientific literature on abortion and women’s mental health. In: MacNair RM. (ed.) Peace psychology perspectives on abortion. Kansas City, MO: Feminism & Nonviolence Studies Association, 2016, pp. 74–93. [ Google Scholar ]
- 137. Hill R. Abortion researcher confounded by study. New Zealand Herald, 1 May 2006, http://www.nzherald.co.nz/nz/news/article.cfm?c_id=1&objectid=10362476
- 138. Fergusson DM, Horwood LJ, Ridder EM. Abortion in young women and subsequent mental health. J Child Psychol Psychiatry Allied Discip 2006; 47(1): 16–24. [ DOI ] [ PubMed ] [ Google Scholar ]
- 139. Speckhard A. Post abortion distress—the politically incorrect trauma. Anne Speckhard, Wordpress.com, 2013, https://annespeckhard.wordpress.com/2013/05/14/post-abortion-distress-the-politically-incorrect-trauma/
- 140. Sobie A. Lead author refuses to release abortion data collected under federal grant. AfterAbortion.org, 13 August 2008, http://afterabortion.org/2008/chair-of-apa-abortion-report-task-force-violates-apa-ethics-rules/
- 141. Reardon DC. Postpartum mental health study flawed by fetal loss omission. Scand J Prim Health Care 2015; 33(4): 318–319. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 142. Baker A. Pro-voice: how to keep listening when the world wants a fight. Oakland, CA: Berrett-Koehler Publishers, Inc, 2015. [ Google Scholar ]
- 143. Laidman J. After decades of research, evaluating abortion’s effect still difficult. Toledo Blade, 22 January 2004, http://www.toledoblade.com/Politics/2004/01/22/After-decades-of-research-evaluating-abortion-s-effect-still-difficult.html
- 144. Russo NF. Response from Div. 35 task force on reproductive issues. Monit Pyschology 2003; 34(4): 4. [ Google Scholar ]
- 145. Major B, Richards C, Cooper ML, et al. Personal resilience, cognitive appraisals, and coping: an integrative model of adjustment to abortion. J Pers Soc Psychol 1998; 74(3): 735–752. [ DOI ] [ PubMed ] [ Google Scholar ]
- 146. Coleman PK, Boswell K, Etzkorn K, et al. Women who suffered emotionally from abortion: a qualitative synthesis of their experiences. J Am Phys Surg 2017; 22(4): 113–118. [ Google Scholar ]
- 147. Cohen BM. Embracing complexity in psychiatric diagnosis, treatment, and research. JAMA Psychiatry 2016; 511(7510): 421–427. [ DOI ] [ PubMed ] [ Google Scholar ]
- 148. Miller WB, Pasta DJ, Dean CL. Testing a model of the psychological consequences of abortion. In: Beckman LJ, Harvey SM. (eds) The new civil war: the psychology, culture, and politics of abortion. Washington, DC: American Psychological Association, 1998, pp. 235–267. [ Google Scholar ]
- 149. Curley M. An explanatory model to guide assessment, risk and diagnosis of psychological distress after abortion. Open J Obstet Gynecol 2014; 4(15): 944–953. [ Google Scholar ]
- 150. Hoekzema E, Barba-Müller E, Pozzobon C, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci 2016; 20: 287–296. [ DOI ] [ PubMed ] [ Google Scholar ]
- 151. Cozzarelli C, Sumer N, Major B. Mental models of attachment and coping with abortion. J Pers Soc Psychol 1998; 74(2): 453–467. [ DOI ] [ PubMed ] [ Google Scholar ]
- 152. Speckhard A, Mufel N. Universal responses to abortion? Attachment, trauma, and grief responses in women following abortion. J Prenat Perinat Psychol 2003; 18: 3–37. [ Google Scholar ]
- 153. Kaij L, Malmquist A, Nilsson Å. Psychiatric aspects of spontaneous abortion—II. The importance of bereavement, attachment and neurosis in early life. J Psychosom Res 1969; 13: 53–59. [ DOI ] [ PubMed ] [ Google Scholar ]
- 154. Allanson S, Astbury J. Attachment style and broken attachments: violence, pregnancy, and abortion. Aust J Psychol 2001; 53: 146–151. [ Google Scholar ]
- 155. Li J, Laursen TM, Precht DH, et al. Hospitalization for mental illness among parents after the death of a child. N Engl J Med 2005; 352(12): 1190–1196. [ DOI ] [ PubMed ] [ Google Scholar ]
- 156. Cacciatore J, Defrain J, Jones KLC. When a baby dies: ambiguity and stillbirth. Marriage Fam Rev 2008; 44(4): 439–454. [ Google Scholar ]
- 157. Keesee NJ, Currier JM, Neimeyer RA. Predictors of grief following the death of one’s child: the contribution of finding meaning. J Clin Psychol 2008; 64(10): 1145–1163. [ DOI ] [ PubMed ] [ Google Scholar ]
- 158. Rubin S, Malkinson R. Parental response to child loss across the life cycle: clinical and research perspectives. In: Stroebe MS, Hansson RO, Stroebe W. (eds) Handbook of bereavement research: consequences, coping, and care. Washington, DC: American Psychological Association, 2001, pp. 219–239. [ Google Scholar ]
- 159. Kersting A, Kroker K, Steinhard J, et al. Complicated grief after traumatic loss: a 14-month follow up study. Eur Arch Psychiatry Clin Neurosci 2007; 257(8): 437–443. [ DOI ] [ PubMed ] [ Google Scholar ]
- 160. Speckhard AP, Rue VP. Complicated mourning: dynamics of impacted post abortion grief. Pre-Peri-Natal Psychol J. 1993; 8(1): 5–32. [ Google Scholar ]
- 161. Lang A, Fleiszer A, Duhamel F. Perinatal loss and parental grief: the challenge of ambiguity and disenfranchised grief. Omega 2011; 63(2): 183–196. [ DOI ] [ PubMed ] [ Google Scholar ]
- 162. Wijngaards-de Meij L, Stroebe M, Schut H, et al. Couples at risk following the death of their child: predictors of grief versus depression. J Consult Clin Psychol 2005; 73(4): 617–623. [ DOI ] [ PubMed ] [ Google Scholar ]
- 163. Lundorff M, Holmgren H, Zachariae R, et al. Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J Affect Disord 2017; 212: 138–149. [ DOI ] [ PubMed ] [ Google Scholar ]
- 164. Betz G, Thorngren J. Ambiguous loss and the family grieving process. Fam J 2006; 14: 359–365. [ Google Scholar ]
- 165. Rosenblatt P, Burns L. Long-term effects of perinatal loss. J Fam Issues 1986; 7: 237–253. [ Google Scholar ]
- 166. Kero A, Lalos A. Ambivalence —a logical response to legal abortion: a prospective study among women and men. J Psychosom Obstet Gynaecol 2000; 21(2): 81–91. [ DOI ] [ PubMed ] [ Google Scholar ]
- 167. Bonanno GA, Papa A, Lalande K, et al. Grief processing and deliberate grief avoidance: a prospective comparison of bereaved spouses and parents in the United States and the People’s Republic of China. J Consult Clin Psychol 2005; 73(1): 86–98. [ DOI ] [ PubMed ] [ Google Scholar ]
- 168. Wojnar DM, Swanson KM, Adolfsson A-S. Confronting the inevitable: a conceptual model of miscarriage for use in clinical Practice and research. Death Stud 2011; 35(6): 536–558. [ DOI ] [ PubMed ] [ Google Scholar ]
- 169. Ney PG, Fung T, Wickett AR, et al. The effects of pregnancy loss on women’s health. Soc Sci Med 1994; 38(9): 1193–1200. [ DOI ] [ PubMed ] [ Google Scholar ]
- 170. Giannandrea SAM, Cerulli C, Anson E, et al. Increased risk for postpartum psychiatric disorders among women with past pregnancy loss. J Womens Health 2013; 22(9): 760–768. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 171. Speckhard AC, Rue VM. Postabortion syndrome: an emerging public health concern. J Soc Issues 1992; 48(3): 95–119. [ Google Scholar ]
- 172. Söderberg H, Janzon L, Sjöberg NO. Emotional distress following induced abortion: a study of its incidence and determinants among abortees in Malmö, Sweden. Eur J Obstet Gynecol Reprod Biol 1998; 79(2): 173–178. [ DOI ] [ PubMed ] [ Google Scholar ]
- 173. Kero A, Högberg U, Lalos A. Wellbeing and mental growth-long-term effects of legal abortion. Soc Sci Med 2004; 58(12): 2559–2569. [ DOI ] [ PubMed ] [ Google Scholar ]
- 174. Söderberg H, Andersson C, Janzon L, et al. Selection bias in a study on how women experienced induced abortion. Eur J Obstet Gynecol Reprod Biol 1998; 77(1): 67–70. [ DOI ] [ PubMed ] [ Google Scholar ]
- 175. Poppema S, Henderson M. Why I am an abortion doctor. New York: Prometheus Books, 1996, 266 pp. [ Google Scholar ]
- 176. McCarthy C. Worst form of birth control hurts woman’s psyche. The Washington Post, 28 February 1971, p. B2. [ Google Scholar ]
- 177. McCarthy C. The real anguish of abortions. The Washington Post, 5 February 1989, https://www.washingtonpost.com/archive/lifestyle/1989/02/05/the-real-anguish-of-abortions/b19f1b34-d561-415d-9974-1774c351cb5c/
- 178. Jenkins N. Hardly any women regret having an abortion, a new study finds. Time, 14 July 2015, p. 10, http://time.com/3956781/women-abortion-regret-reproductive-health/ (accessed 28 December 2016).
- 179. Rocca CH, Kimport K, Roberts SCM, et al. Decision rightness and emotional responses to abortion in the United States: a longitudinal study. PLoS ONE 2015; 10(7): e0128832. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 180. Dreaper J. Abortion “does not raise” mental health risk. BBC News, 2011, http://www.bbc.com/news/health-16094906 (accessed 28 December 2016).
- 181. Reardon DC. Aborted women, silent no more. Chicago, IL: Loyola University Press, 1987, 373 pp. [ Google Scholar ]
- 182. Dykes K, Slade P, Haywood A. Long term follow-up of emotional experiences after termination of pregnancy: women’s views at menopause. J Reprod Infant Psychol 2011; 29(1): 93–112. [ Google Scholar ]
- 183. Reardon DC, Ney PG. Abortion and subsequent substance abuse. Am J Drug Alcohol Abuse 2000; 26(1): 61–75. [ DOI ] [ PubMed ] [ Google Scholar ]
- 184. Reardon DC, Cougle JR. Depression and unintended pregnancy in young women. BMJ 2002; 324(7345): 1097. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 185. Jones EF, Forrest JD. Underreporting of abortion in surveys of U.S. women: 1976 to 1988. Demography 1992; 29(1): 113–126. [ PubMed ] [ Google Scholar ]
- 186. Jones RK, Kost K. Underreporting of induced and spontaneous abortion in the United States: an analysis of the 2002 National Survey of Family Growth. Stud Fam Plann 2007; 38(3): 187–197. [ DOI ] [ PubMed ] [ Google Scholar ]
- 187. van Ditzhuijzen J, ten Have M, de Graaf R, et al. Psychiatric history of women who have had an abortion. J Psychiatr Res 2013; 47(11): 1737–1743. [ DOI ] [ PubMed ] [ Google Scholar ]
- 188. Biggs MA, Upadhyay UD, McCulloch CE, et al. Women’s mental health and well-being 5 years after receiving or being denied an abortion: a prospective, longitudinal cohort study. JAMA Psychiatry 2017; 74: 169–178. [ DOI ] [ PubMed ] [ Google Scholar ]
- 189. Ingraham C. 95 percent of women who’ve had an abortion say it was the right decision. The Washington Post, 14 July 2015, https://www.washingtonpost.com/news/wonk/wp/2015/07/14/95-percent-of-women-whove-had-an-abortion-say-it-was-the-right-decision/
- 190. Adler NE. Sample attrition in studies of psychosocial sequelae of abortion: how great a problem? J Appl Soc Psychol 1976; 6(3): 240–259. [ Google Scholar ]
- 191. Weisæth L. Importance of high response rates in traumatic stress research. Acta Psychiatr Scand 1989; 355: 131–137. [ PubMed ] [ Google Scholar ]
- 192. Romans S. Asking the unanswerable: stymied again by the impossibility of sensible controls. Aust N Z J Psychiatry 2013; 47(9): 802–804. [ DOI ] [ PubMed ] [ Google Scholar ]
- 193. Fergusson DM, Horwood LJ, Boden JM. Abortion and mental health: a response to Romans and Steinberg. Aust N Z J Psychiatry 2013; 47(12): 1201–1203. [ DOI ] [ PubMed ] [ Google Scholar ]
- 194. Stotland NL, Shrestha AD. More evidence that abortion is not associated with increased risk of mental illness. JAMA Psychiatry 2018; 75: 775–776. [ DOI ] [ PubMed ] [ Google Scholar ]
- 195. Karalis E, Ulander V-M, Tapper A-M, et al. Decreasing mortality during pregnancy and for a year after while mortality after termination of pregnancy remains high: a population-based register study of pregnancy-associated deaths in Finland 2001-2012. BJOG 2017; 124: 1115–1121. [ DOI ] [ PubMed ] [ Google Scholar ]
- 196. Gissler M, Berg C, Bouvier-Colle M-H, et al. Injury deaths, suicides and homicides associated with pregnancy, Finland 1987-2000. Eur J Public Health 2005; 15(5): 459–463. [ DOI ] [ PubMed ] [ Google Scholar ]
- 197. Shapiro GD, Séguin JR, Muckle G, et al. Previous pregnancy outcomes and subsequent pregnancy anxiety in a Quebec prospective cohort. J Psychosom Obstet Gynaecol 2017; 38(2): 121–132. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 198. Reardon DC. The embrace of the pro-abortion turnaway study. Wishful thinking? or willful deceptions? Linacre Q 2018; 85(3): 204–212. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 199. Petersen R, Moos M-K. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues 1997; 7(4): 234–240. [ DOI ] [ PubMed ] [ Google Scholar ]
- 200. Finer L, Zolna M. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health 2014; 104(Suppl. 1): S43–S48. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 201. Russo N, Zierk K. Abortion, childbearing, and women’s well-being. Prof Psychol Res 1992; 23: 269–280. [ Google Scholar ]
- 202. Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa, ON, Canada: Department of Epidemiology and Community Medicine, University of Ottawa, http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [ Google Scholar ]
- 203. Reardon DC, Thorp JM. Pregnancy associated death in record linkage studies relative to delivery, termination of pregnancy, and natural losses: a systematic review with a narrative synthesis and meta-analysis. SAGE Open Med 2017; 5: 205031211774049. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 204. Curley M, Johnston C. The characteristics and severity of psychological distress after abortion among university students. J Behav Heal Serv Res 2013; 40(3): 279–293. [ DOI ] [ PubMed ] [ Google Scholar ]
- 205. Galbally M, Lewis AJ, Ijzendoorn Mv, et al. The role of oxytocin in mother-infant relations: a systematic review of human studies. Harv Rev Psychiatry 2011; 19(1): 1–14. [ DOI ] [ PubMed ] [ Google Scholar ]
- 206. Kleinman JC, Kovar MG, Feldman JJ, et al. A comparison of 1960 and 1973-1974 early neonatal mortality in selected states. Am J Epidemiol 1978; 108(6): 454–469. [ DOI ] [ PubMed ] [ Google Scholar ]
- 207. Grace JT. Development of maternal-fetal attachment during pregnancy. Nurs Res 2017; 38(4): 228–232. [ PubMed ] [ Google Scholar ]
- 208. Munk-Olsen T, Gasse C, Laursen TM. Prevalence of antidepressant use and contacts with psychiatrists and psychologists in pregnant and postpartum women. Acta Psychiatr Scand 2012; 125(4): 318–324. [ DOI ] [ PubMed ] [ Google Scholar ]
- 209. Munk-Olsen T, Maegbaek ML, Johannsen BM, et al. Perinatal psychiatric episodes: a population-based study on treatment incidence and prevalence. Transl Psychiatry 2016; 6(10): e919. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 210. Munk-Olsen T, Pedersen HS, Laursen TM, et al. Use of primary health care prior to a postpartum psychiatric episode. Scand J Prim Health Care 2015; 33(2): 127–133. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 211. Kumar R, Robson K. Previous induced abortion and ante-natal depression in primiparae: preliminary report of a survey of mental health in pregnancy. Psychol Med 1978; 8(4): 711–715. [ DOI ] [ PubMed ] [ Google Scholar ]
- 212. McCarthy F, Moss-Morris R, Khashan A, et al. Previous pregnancy loss has an adverse impact on distress and behaviour in subsequent pregnancy. BJOG 2015; 122(13): 1757–1764. [ DOI ] [ PubMed ] [ Google Scholar ]
- 213. Bradley CF. Abortion and subsequent pregnancy. Can J Psychiatry 1984; 29(6): 494–498. [ DOI ] [ PubMed ] [ Google Scholar ]
- 214. Kitamura T, Shima S, Sugawara M, et al. Psychological and social correlates of the onset of affective disorders among pregnant women. Psychol Med 1993; 23(4): 967–975. [ DOI ] [ PubMed ] [ Google Scholar ]
- 215. Devore NE. The relationship between previous elective abortions and postpartum depressive reactions. JOGN Nurs 1979; 8(4): 237–240. [ DOI ] [ PubMed ] [ Google Scholar ]
- 216. Huang Z, Hao J, Su P, et al. The impact of prior abortion on anxiety and depression symptoms during a subsequent pregnancy: data from a population-based cohort study in China. Bull Clin Psychopharmacol 2012; 22(11): 51–58. [ Google Scholar ]
- 217. Munk-Olsen T, Bech BH, Vestergaard M, et al. Psychiatric disorders following fetal death: a population-based cohort study. BMJ Open 2014; 4: e005187. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 218. Waqas A, Raza N, Lodhi HW, et al. Psychosocial factors of antenatal anxiety and depression in Pakistan: is social support a mediator? PLoS ONE 2015; 10(1): e0116510. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 219. Ali NS, Azam IS, Ali BS, et al. Frequency and associated factors for anxiety and depression in pregnant women: a hospital-based cross-sectional study. Sci World J 2012; 2012: 653098. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 220. Ajinkya S, Jadhav PR, Srivastava NN. Depression during pregnancy: prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J 2013; 22(1): 37–40. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 221. Faisal-Cury A, Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Ment Health 2007; 10(1): 25–32. [ DOI ] [ PubMed ] [ Google Scholar ]
- 222. Chojenta C, Harris S, Reilly N, et al. History of pregnancy loss increases the risk of mental health problems in subsequent pregnancies but not in the postpartum. PLoS ONE 2014; 9(4): e95038. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 223. Al-Shami N, Moawed SEA. Identification of factors associated with postpartum depression among Saudi females in Riyadh City, 2010, http://repository.ksu.edu.sa/jspui/handle/123456789/19373 (accessed 3 January 2017).
- 224. Räisänen S, Lehto SM, Nielsen HS, et al. Fear of childbirth predicts postpartum depression: a population-based analysis of 511 422 singleton births in Finland. BMJ Open 2013; 3(11): e004047. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 225. Montmasson H, Bertrand P, Perrotin F, et al. Facteurs prédictifs de l’état de stress post-traumatique du postpartum chez la primipare. J Gynécologie Obs Biol la Reprod 2012; 41(6): 553–560. [ DOI ] [ PubMed ] [ Google Scholar ]
- 226. Kumar R, Robson KM. A prospective study of emotional disorders in childbearing women. Br J Psychiatry 1984; 144: 35–47. [ DOI ] [ PubMed ] [ Google Scholar ]
- 227. Reardon DC. Lack of pregnancy loss history mars depression study. Acta Psychiatr Scand 2012; 126(2): 155. [ DOI ] [ PubMed ] [ Google Scholar ]
- 228. Afable-Munsuz A, Speizer I, Magnus JH, et al. A positive orientation toward early motherhood is associated with unintended pregnancy among New Orleans youth. Matern Child Health J 2006; 10(3): 265–276. [ DOI ] [ PubMed ] [ Google Scholar ]
- 229. Ney PG. Some real issues surrounding abortion, or, the current practice of abortion is unscientific. J Clin Ethics 1993; 4(2): 179–180. [ PubMed ] [ Google Scholar ]
- 230. Ulene V. Life with Lasik: a closer look. Los Angeles Times, 16 June 2008, http://articles.latimes.com/2008/jun/16/health/he-themd16
- 231. Murphy JF, O’Driscoll K. Therapeutic abortion: the medical argument. Ir Med J 1982; 75(8): 304–306. [ PubMed ] [ Google Scholar ]
- 232. Reardon DC, Strahan TW, Thorp JM, et al. Deaths associated with abortion compared to childbirth —a review of new and old data and the medical and legal implications. J Contemp Health Law Policy 2004; 20(2): 279–327. [ PubMed ] [ Google Scholar ]
- 233. Calhoun BC. Induced abortion and risk of later premature births. J Am Phys Surg 2003; 8(2): 46–49. [ Google Scholar ]
- 234. 8th Cir. (en banc). Planned Parenthood Minn., N.D., S.D. v. Rounds, 2012. [ Google Scholar ]
- 235. United Nations. Beijing declaration and platform for action. In: Adopted at the fourth world conference on women, Beijing, China, 4–15 September 1995. [ Google Scholar ]
- 236. Bradford-Hill A. The environment and disease: association or causation? Proc R Soc Med 1965; 58: 295–300. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 237. Biggs MA, Neuhaus JM, Foster DG. Mental health diagnoses 3 years after receiving or being denied an abortion in the United States. Am J Public Health 2015; 105(12): 2557–2563. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 238. Sriarporn P, Turale S, Lordee N, et al. Support program for women suffering grief after termination of pregnancy: a pilot study. Nurs Heal Sci 2017; 19(1): 75–80. [ DOI ] [ PubMed ] [ Google Scholar ]
- 239. Ney PG, Ball K, Sheils C. Results of group psychotherapy for abuse, neglect and pregnancy loss. Curr Womens Health Rev 2010; 6(4): 332–340. [ Google Scholar ]
- 240. Jaramillo S. Mending broken lives: post-abortion healing. Virginia Beach, VA: Regent University, 2017. [ Google Scholar ]
- 241. Artist hanged herself after aborting her twins. The Telegraph, 22 February 2008, http://www.telegraph.co.uk/news/uknews/1579455/Artist-hanged-herself-after-aborting-her-twins.html (accessed 31 March 2016).
- 242. Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet 2010; 375(9726): 1609–1623. [ DOI ] [ PubMed ] [ Google Scholar ]
- 243. Herman JL. Trauma and recovery: the aftermath of violence —from domestic abuse to political terror. New York: Basic Books, 1992. [ Google Scholar ]
- 244. Duhaime L. Thin skull rule definition. Duhaime’s Law Dictionary, 2016, http://www.duhaime.org/LegalDictionary/T/ThinSkullRule.aspx
- 245. Needle RB, Walker LE. Abortion counseling: a clinician’s guide to psychology, legislation, politics, and competency. New York, NY: Springer Publishing Company, 2007. [ Google Scholar ]
- 246. Gissler M, Hemminki E. Pregnancy-related violent deaths. Scand J Public Health 1999; 27: 54–55. [ PubMed ] [ Google Scholar ]
- 247. Taft AJ, Watson LF, Lee C. Violence against young Australian women and association with reproductive events: a cross-sectional analysis of a national population sample. Aust N Z J Public Health 2004; 28(4): 324–329. [ DOI ] [ PubMed ] [ Google Scholar ]
- 248. Russo NF. Abortion, unwanted childbearing, and mental health. Salud Ment 2014; 37(4): 283–291. [ Google Scholar ]
- 249. Shuping M. Risk factors. In: MacNair RM. (ed.) Peace psychology perspectives on abortion. Kansas City, MO: Feminism & Nonviolence Studies Association, 2016, pp. 94–114. [ Google Scholar ]
- 250. Reardon D, Makimma J, Sobie A. (eds). Victims and victors: speaking out about their pregnancies, abortions, and children resulting from sexual assault. Springfield, IL: Acorn Books, 2000, 192 pp. [ Google Scholar ]
- 251. Robinson GE, Stotland NL, Russo NF, et al. Is there an “abortion trauma syndrome”? Critiquing the evidence. Harv Rev Psychiatry 2009; 17(4): 268–290. [ DOI ] [ PubMed ] [ Google Scholar ]
- 252. Stotland NL. The myth of the abortion trauma syndrome. JAMA J Am Med Assoc 1992; 268(15): 2078–2079. [ PubMed ] [ Google Scholar ]
- 253. Sentilhes L, Maillard F, Brun S, et al. Risk factors for chronic post-traumatic stress disorder development one year after vaginal delivery: a prospective, observational study. Sci Rep 2017; 7(1): 8724. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 254. Mahmoodi Z, Dolatian M, Shaban Z, et al. Correlation between kind of delivery and posttraumatic stress disorder. Ann Med Health Sci Res 2016; 6(6): 356–361. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 255. Dikmen-Yildiz P, Ayers S, Phillips L. Longitudinal trajectories of post-traumatic stress disorder (PTSD) after birth and associated risk factors. J Affect Disord 2018; 229: 377–385. [ DOI ] [ PubMed ] [ Google Scholar ]
- 256. Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res 1996; 40(3): 235–244. [ DOI ] [ PubMed ] [ Google Scholar ]
- 257. Farren J, Jalmbrant M, Ameye L, et al. Post-traumatic stress, anxiety and depression following miscarriage or ectopic pregnancy: a prospective cohort study. BMJ Open 2016; 6(11): e011864. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 258. Krosch DJ, Shakespeare-Finch J. Grief, traumatic stress, and posttraumatic growth in women who have experienced pregnancy loss. Psychol Trauma 2017; 9(4): 425–433. [ DOI ] [ PubMed ] [ Google Scholar ]
- 259. Coleman PK, Coyle CT, Rue VM. Late-term elective abortion and susceptibility to posttraumatic stress symptoms. J Pregnancy 2010; 2010: 130519. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 260. Hamama L, Rauch SA, Sperlich M, et al. Previous experience of spontaneous or elective abortion and risk for posttraumatic stress and depression during subsequent pregnancy. Depress Anxiety 2010; 27(8): 699–707. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 261. Kersting A, Kroker K, Steinhard J, et al. Psychological impact on women after second and third trimester termination of pregnancy due to fetal anomalies versus women after preterm birth-a 14-month follow up study. Arch Womens Ment Health 2009; 12(4): 193–201. [ DOI ] [ PubMed ] [ Google Scholar ]
- 262. Kelly T, Suddes J, Howel D, et al. Comparing medical versus surgical termination of pregnancy at 13-20 weeks of gestation: a randomised controlled trial. BJOG 2010; 117(12): 1512–1520. [ DOI ] [ PubMed ] [ Google Scholar ]
- 263. Borins EFM, Forsythe PJ. Past trauma and present functioning of patients attending a women’s psychiatric clinic. Am J Psychiatry 1985; 142(4): 460–463. [ DOI ] [ PubMed ] [ Google Scholar ]
- 264. Fisch RZ, Tadmor O. Iatrogenic post-traumatic stress disorder. Lancet 1989; 2(8676): 1397. [ DOI ] [ PubMed ] [ Google Scholar ]
- 265. Vukelić J, Kapamadzija A, Kondić B. Investigation of risk factors for acute stress reaction following induced abortion. Med Pregl 2018; 63(5–6): 399–403. [ DOI ] [ PubMed ] [ Google Scholar ]
- 266. Wallin Lundell I, Sundström Poromaa I, Ekselius L, et al. Neuroticism-related personality traits are associated with posttraumatic stress after abortion: findings from a Swedish multi-center cohort study. BMC Womens Health 2017; 17(1): 96. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 267. Zulčić-Nakić V, Pajević I, Hasanović M, et al. Psychological problems sequalae in adolescents after artificial abortion. J Pediatr Adolesc Gynecol 2012; 25(4): 241–247. [ DOI ] [ PubMed ] [ Google Scholar ]
- 268. Suliman S, Ericksen T, Labuschgne P, et al. Comparison of pain, cortisol levels, and psychological distress in women undergoing surgical termination of pregnancy under local anaesthesia versus intravenous sedation. BMC Psychiatry 2007; 7: 24. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 269. Rousset C, Brulfert C, Séjourné N, et al. Posttraumatic stress disorder and psychological distress following medical and surgical abortion. J Reprod Infant Psychol 2011; 29(5): 506–517. [ Google Scholar ]
- 270. Gravensteen IK, Helgadóttir LB, Jacobsen E-M, et al. Women’s experiences in relation to stillbirth and risk factors for long-term post-traumatic stress symptoms: a retrospective study. BMJ Open 2013; 3(10): e003323. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 271. Ryan GL, Mengeling MA, Booth BM, et al. Voluntary and involuntary childlessness in female veterans: associations with sexual assault. Fertil Steril 2014; 102(2): 539–547. [ DOI ] [ PubMed ] [ Google Scholar ]
- 272. Fergusson DM. Abortion and mental health. Psychiatr Bull 2008; 32(9): 321–324. [ Google Scholar ]
- 273. Great Britain Commission of Inquiry into the Operation and Consequences of The Abortion Act. The physical and psycho-social effects of abortion on women. London: Great Britain, Parliament, House of Lords, Commission of Inquiry into the Operation and Consequences of The Abortion Act, 1994. [ Google Scholar ]
- 274. National Collaborating Centre for Mental Health. Induced abortion and mental health systematic review consultation—6 April to 29 June 2011 comments and responses. London: Academy of Medical Royal Colleges, 2011, https://www.scribd.com/document/327608591/Induced-Abortion-and-Mental-Health-Systematic-Review-Consultation-6-April-to-29-June-2011-Comments-and-Responses [ Google Scholar ]
- 275. Coleman P, Speckhard A, Ney P, et al. NCCMH review. AbortionRisks.org, 2017, http://abortionrisks.org/index.php?title=NCCMH_Review (accessed 8 February2017).
- 276. Morey RD, Chambers CD, Etchells PJ, et al. The Peer Reviewers’ Openness Initiative: incentivizing open research practices through peer review. R Soc Open Sci 2016; 3(1): 150547. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 277. Schofield PN, Bubela T, Weaver T, et al. Post-publication sharing of data and tools. Nature 2009; 461(7261): 171–173. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 278. American Psychological Association. Ethical principles of psychologists and code of conduct, 2010, http://www.apa.org/ethics/code/index.aspx#8_14 (accessed 2 February 2017).
- 279. Wicherts JM, Borsboom D, Kats J, et al. The poor availability of psychological research data for reanalysis. Am Psychol 2006; 61(7): 726–728. [ DOI ] [ PubMed ] [ Google Scholar ]
- 280. Vanpaemel W, Vermorgen M, Deriemaecker L, et al. Are we wasting a good crisis? The availability of psychological research data after the storm. Collabra 2015; 1(1): 3. [ Google Scholar ]
- 281. Naik G. Peer-review activists push psychology journals towards open data. Nature 2017; 543: 161. [ DOI ] [ PubMed ] [ Google Scholar ]
- 282. Reardon DC, Coleman PK. Munk-Olsen et al. AbortionRisks.org, 2017, http://abortionrisks.org/index.php?title=Munk-Olsen_et_al (accessed 2 February 2017).
- 283. Munk-Olsen T, Laursen TM, Meltzer-Brody S, et al. Psychiatric disorders with postpartum onset: possible early manifestations of bipolar affective disorders. Arch Gen Psychiatry 2012; 69: 428–434. [ DOI ] [ PubMed ] [ Google Scholar ]
- 284. Munk-Olsen T, Agerbo E. Does childbirth cause psychiatric disorders? A population-based study paralleling a natural experiment. Epidemiology 2015; 26(1): 79–84. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 285. Blackmore ER, Côté-Arsenault D, Tang W, et al. Previous prenatal loss as a predictor of perinatal depression and anxiety. Br J Psychiatry 2011; 198(5): 373–378. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 286. Räisänen S, Lehto SM, Nielsen HS, et al. Risk factors for and perinatal outcomes of major depression during pregnancy: a population-based analysis during 2002-2010 in Finland. BMJ Open 2014; 4(11): e004883. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 287. Marengo E, Martino DJ, Igoa A, et al. Unplanned pregnancies and reproductive health among women with bipolar disorder. J Affect Disord 2015; 178: 201–205. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (4.5 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM

Add to Collections
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 02 January 2024
Psychological traits and public attitudes towards abortion: the role of empathy, locus of control, and need for cognition
- Jiuqing Cheng 1 ,
- Ping Xu 2 &
- Chloe Thostenson 1
Humanities and Social Sciences Communications volume 11 , Article number: 23 ( 2024 ) Cite this article
4675 Accesses
1 Altmetric
Metrics details
- Social policy
In the summer of 2022, the U.S. Supreme Court overturned the historic Roe v. Wade ruling, prompting various states to put forth ballot measures regarding state-level abortion rights. While earlier studies have established associations between demographics, such as religious beliefs and political ideologies, and attitudes toward abortion, the current research delves into the role of psychological traits such as empathy, locus of control, and need for cognition. A sample of 294 U.S. adults was obtained via Amazon Mechanical Turk, and participants were asked to provide their attitudes on seven abortion scenarios. They also responded to scales measuring empathy toward the pregnant woman and the unborn, locus of control, and need for cognition. Principal Component Analysis divided abortion attitudes into two categories: traumatic abortions (e.g., pregnancies due to rape) and elective abortions (e.g., the woman does not want the child anymore). After controlling for religious belief and political ideology, the study found psychological factors accounted for substantial variation in abortion attitudes. Notably, empathy toward the pregnant woman correlated positively with abortion support across both categories, while empathy toward the unborn revealed an inverse relationship. An internal locus of control was positively linked to support for both types of abortions. Conversely, external locus of control and need for cognition only positively correlated with attitudes toward elective abortion, showing no association with traumatic abortion attitudes. Collectively, these findings underscore the significant and unique role psychological factors play in shaping public attitudes toward abortion. Implications for research and practice were discussed.
Similar content being viewed by others
Death anxiety as mediator of relationship between renunciation of desire and mental health as predicted by Nonself Theory
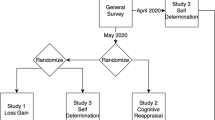
The Psychological Science Accelerator’s COVID-19 rapid-response dataset
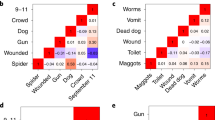
Conservatives and liberals have similar physiological responses to threats
The U.S. Supreme Court overturned the long-time landmark ruling of Roe v. Wade in 2022 summer. Debates and legal challenges regarding legal abortion in the U.S. have been heated (Felix et al., 2023 ). Furthermore, residents in several states have or will cast their vote on a ballot measure to determine abortion rights at the state level. A Gallup poll released in 2023 summer found that about one third of voters indicated that they would only vote for a candidate who shared their views on abortion (Saad, 2023 ). Therefore, it is imperative to understand people’s attitudes toward abortion. Past research on such attitudes have mainly focused on the role of political ideology and religious belief (e.g., Hess and Rueb, 2005 ); however, to our knowledge, relatively few studies have been done to examine the psychological underpinnings. Here we propose that examining the correlations between psychological factors and attitudes toward abortion has the potential to make contributions from the perspectives of both research and practice.
First, compared to attitudes in everyday life such as attitudes toward a product or brand, attitudes toward abortion are unique because it often elicits strong emotional response and conflict experience (Foster et al., 2012 ; Scott, 1989 ). Moreover, such an attitude goes beyond individual preference as it is deeply intertwined with one’s moral and religious beliefs, cultural background, and societal norms. Debate on abortion is not merely about a personal choice; it is about the definitions of life, rights, and autonomy (Osborne et al., 2022 ; Scott, 1989 ). For abortion, the contrasting views may lead to polarized opinions. In contrast, disagreements about a product or brand preference are typically less emotionally charged and do not carry the same societal weight. Therefore, given the unique nature of attitudes toward abortion as described above, it remains unclear whether psychological factors that correlate with attitudes in other areas still apply and, if so, in what capacity they do so. Additionally, as introduced below, several studies in this area employed a qualitative approach (interview). While the qualitative approach offered valuable insights into individuals’ perspectives on abortion, we aim to expand upon these findings by employing a quantitative approach. Especially, the quantitative approach allows us to explore the unique relationship between psychology and abortion attitudes after statistically controlling for other powerful factors like religious belief and political ideology. Together, a major goal of the present study is to provide initial empirical evidence for the correlations between attitudes toward abortion and certain psychological factors. We will further detail how our study might fill research gaps when introducing specific psychological factors as described below.
Second, examining the correlations between psychological factors and attitudes toward abortion may also offer practical insights. Consider the role of thinking style, for instance. The decision to pursue an abortion is imperative and often a prominently salient one, impacting not just the pregnant woman but also her family and extensive social network. Such a decision is complex and challenging due to intense feelings (e.g., conflict) and the balance between a woman’s bodily autonomy and fetal rights. From this viewpoint, there might be a correlation between attitudes toward abortion and one’s thinking style, especially their willingness to address complex and difficult issues. Past research has highlighted the connection between rational decision-making and the availability of relevant information (Shafir and LeBoeuf, 2002 ). Hence, to facilitate informed decisions, comprehensive knowledge about abortion is both essential and beneficial. The present study will examine the relationship between thinking style and abortion attitudes. Should a correlation be identified, our study would suggest individuals engage more deeply in critical thinking about the issues of abortion to enhance abortion-related education and informed decision-making.
Together, the present study aims to shed more light on the unique role of psychology in abortion attitudes, particularly in the presence of political ideology and religious belief. Specifically, we choose to examine the factors of empathy, locus of control, and thinking style (need for cognition) based on three considerations. Firstly, from a face validity perspective, the psychological constructs are predicted to exhibit a relationship with abortion attitudes. For example, the internal locus of control aligns well with the pro-choice mantra, ‘my body, my choice. Secondly, as detailed below, although these constructs have been explored in previous studies, they have only received limited attention and their relations with abortion attitudes remain inconclusive. Hence, our study aims to fill the gaps from past research by further clarifying their roles in attitudes toward abortion. Thirdly, research has indicated significant intersections between elements like cognitive style, empathy, and locus of control with various decisions, especially in health contexts (Marton et al., 2021 ; Pfattheicher et al., 2020 ; Xu and Cheng, 2021 ). These elements are tied to motivation, information analysis, and make trade-offs (Fischhoff and Broomell, 2020 ). Building on this, our study seeks to explore the applicability of these factors to the deeply sensitive and polarizing decision of abortion. On the other hand, it is worth noting that the psychological factors examined in our study are not exhaustive or driven by theoretical considerations. However, as mentioned in recent publications (Osborne et al., 2022 ; Valdez et al., 2022 ), past research on abortion attitudes with a psychological perspective is still limited. Therefore, our hope is that the present study could provide initial yet meaningful empirical evidence to exhibit the sophisticated role of psychology in attitudes toward abortion. We detail our rationales for each factor below.
Empathy refers to a variety of cognitive and affective responses, including sharing and understanding, toward others’ experiences (Pfattheicher et al., 2020 ). Previous studies have demonstrated a positive association between empathy and prosocial behaviors, such as caring for others (Moudatsou et al., 2020 ; Klimecki et al., 2016 ), as well as a reduction in conflict and stigma (Batson et al., 1997 ; Klimecki, 2019 ). Recently, Pfattheicher et al. ( 2020 ) also demonstrated that inducing empathy for the vulnerable people could promote taking preventative measures during the Covid-19 pandemic. While researchers advocated for incorporating empathy into abortion-related mental health intervention (Brown et al., 2022 ), the role of empathy in attitudes toward abortion remains understudied. Hunt ( 2019 ) investigated the impact of empathy toward pregnant women by presenting testimonial videos in which a pregnant woman described the challenges she faced due to legal abortion restrictions in Arkansas. However, this manipulation did not significantly reduce participants’ support for the abortion restrictions. Research has found that people’s views on abortion tends to be stable over time (Jelen and Wilcox, 2003 ; Pew Research Center, 2022 ). Hence, a short video used in Hunt ( 2019 ) might not be able to change people’s long-held views on abortion. Instead, we here hypothesize that the pre-existing but not temporality induced empathy play a role in abortion attitudes.
Furthermore, in addition to the empathy toward pregnant woman, it is also reasonable to assume that (some) people may feel empathy toward the unborn. For instance, interviews with Protestant religious leaders exhibited empathy toward both pregnant women and unborn (Dozier et al., 2020 ). Embree ( 1998 ) asked participants to indicate their opinions when responding to different scenarios of abortion. As a result, the study found that 64% and 17% of participants showed a moderate and strong level of empathy for the unborn, respectively. Despite the informative findings, the relationship between attitudes toward abortion and empathy toward the unborn remains unclear, particularly when taking empathy toward pregnant woman and other factors (e.g., political ideology) into account.
Together, we raise three hypotheses regarding the role of empathy as shown below.
H1a: Empathy toward pregnant woman and unborn can coexist.
H1b: People’s empathy toward pregnant woman are positively related to the support toward abortion.
H1c: People’s empathy toward unborn are negatively related to the support toward abortion.
As empathy has been highlighted in the intervention process when dealing with abortion-related mental health issues (Brown et al., 2022 ; Whitaker et al., 2015 ), we hope our findings could generate implications for future research and practice.
Locus of control
Locus of control (LOC) refers to people’s beliefs regarding whether their life outcomes are controlled and determined by their own (internal LOC) or external resources (fate, chance and/or powerful people, external LOC) (Levenson, 1981 ). Before delving into details, it is important to note that the internal and external LOC refer to different dimensions and are not mutually exclusive (Levenson, 1981 ; Reknes et al., 2019 ). For example, a person’s success may be determined by both hardworking and support from others. Regarding abortion attitudes, Sundstrom et al. ( 2018 ) analyzed interview contents and found that some women’s thoughts on pregnancy and abortion aligned with an internal locus of control (e.g., “As women, we need to take control as much as possible of our reproductive health”), while others aligned with an external locus of control (e.g., “leave it in God’s hands…we’ll just play it by ear and if I get pregnant, I get pregnant”).
The findings from Sundstrom et al. ( 2018 ) were informative and consistent with common sense. For example, at face value level, the slogan of “my body my choice” well aligns with the concept of internal LOC. However, the role of internal LOC in abortion attitudes may be more complicated. That is, religious belief may complicate the association between internal LOC and abortion attitudes. Past studies, including a meta-analysis and a study with over 20,000 participants, found a positive relationship between internal LOC and religious belief (Coursey et al., 2013 ; Falkowski, 2000 ; Iles-Caven et al., 2020 ). As noted in these articles, there are similarities between internal LOC and religious belief. For instance, religious beliefs often provide individuals with a sense of meaning, purpose, and guidance in life. Meanwhile, people higher in internal LOC are more likely to report higher levels of existential well-being and purpose in life, which can be associated with religious belief and engagement (Kim-Prieto et al., 2005 ; Krause and Hayward, 2013 ). Thus, the relationship between internal LOC and religious belief may complicate how internal LOC is involved in the abortion attitudes. Sundstrom et al. ( 2018 ) used interviews to explore the role of LOC in thoughts about abortion. However, this method might not sufficiently differentiate the influence of religious beliefs. In this study, we adopt a quantitative approach, using a classical scale to measure LOC. We aim to empirically assess the relationship between internal LOC and attitudes toward abortion, especially when accounting for religious belief. Furthermore, considering that the relationship between internal LOC and abortion attitudes might be intertwined with religious beliefs, we refrain from positing a specific hypothesis at this point.
External LOC, on the other hand, does not appear to have a significant relationship with religious belief. Additionally, a few studies found that people higher in external LOC tended to attribute outcomes to external reasons (Falkowski, 2000 ; Reknes et al., 2019 ). Building on this concept, individuals with a higher external locus of control (LOC) may be more inclined to attribute pregnancy to external factors and place less emphasis on personal responsibility. Accordingly, we predict the hypothesis below.
H2: External LOC will be positively related to the support toward abortion.
Need for cognition
Based on face validity, thinking style might pertain to one’s perception of abortion. For instance, individuals who prioritize comprehensive and empirical data might arrive at a different conclusion than those who lean on personal stories and emotional narratives. A few studies have tapped into the relationship between thinking style and attitudes toward abortion. Valdez et al. ( 2022 ) conducted qualitative interviews on abortion and employed natural language processing techniques to analyze the interviews. The study identified analytical thinking, which involved considering abortion from multiple perspectives, had a negative relationship with the number of cognitive distortions (such as polarized and rigid thinking about abortion). However, such a finding conflicted with another study by Hill ( 2004 ) where the concept of cognitive complexity (thinking beyond surface-level observations) did not correlate with attitudes toward abortion. The inconsistency might be due to methodological issues. For example, the correlations described above in Valdez et al. ( 2022 ) were derived from a small sample consisting of 16 participants. A low reliability of the cognitive complexity scale used in Hill ( 2004 ) might (partly) address the non-significant relationship. Thus, the present study will utilize the Need for Cognition scale, a widely recognized and validated instrument that measures thinking style, to examine its correlation with attitudes toward abortion in a larger sample.
Need for cognition (NFC) pertains to the inclination to derive satisfaction from and actively participate in effortful thinking (Cacioppo et al., 1984 ). Consistent with its concept, past research demonstrated that NFC was positively correlated with information seeking (Verplanken et al., 1992 ), academic achievement (Richardson et al., 2012 ), and logical reasoning performance (Ding et al., 2020 ). As for attitudes toward abortion, we hypothesize the following.
H3: There will be a positive correlation between NFC and attitudes toward abortion.
Our prediction is based on two reasons. First, NFC drives individuals to actively seek and update information and knowledge. It was discovered that acquiring a deeper understanding of abortion correlated with increased support for it (Hunt, 2019 ; Mollen et al., 2018 ). Second and relatedly, NFC was found to be negatively associated with various stereotype memories and positively related to non-prejudicial social judgments (Crawford and Skowronski, 1998 ; Curşeu and de Jong, 2017 ).
In sum, the present study aims to provide empirical evidence for the association between attitudes toward abortion and psychology by examining and clarifying the role of empathy, locus of control, and need for cognition. Past research has repeatedly found the involvement of political ideology and religious belief in abortion attitudes (e.g., Hess and Rueb, 2005 ; Holman et al., 2020 ; Jelen, 2017 ; Osborne et al., 2022 ; Prusaczyk and Hodson, 2018 ). Given their powerful and robust effect, it is crucial to gather additional empirical evidence to elucidate the distinct contribution of psychology to attitudes toward abortion, while considering the influence of political ideology and religious beliefs. Additionally, when describing attitudes toward abortion, the dichotomization of “pro-choice” and “pro-life” have been widely used for decades. However, some studies have criticized that the dichotomization oversimplified attitudes toward abortion (Hunt, 2019 ; Osborne et al., 2022 ; Rye and Underhill, 2020 ). That is, people’s views on abortion vary across different scenarios and reasons. For instance, people showed less support toward abortion with elective reasons than with traumatic reasons (Hoffmann and Johnson, 2005 ). With confirmatory analysis, Osborne et al. ( 2022 ) derived two types of abortion: traumatic (e.g., pregnancy due to rape) vs. elective (e.g., the woman does not want the child anymore). Building on prior research, the current study aims exploring potential variations in attitudes across different abortion reasons. Furthermore, we also intend to examine whether the psychological factors described above have varying associations with different types of abortion.
Participants
The study was approved by IRB before data collection. Participants were recruited from Amazon Mechanical Turk (mTurk) on October 20th, 2022. To be eligible for the study, participants must be an adult, a U.S. citizen, and have an approval rating greater than 98% in mTurk. A total of 300 participants were enrolled into the study. Each participant received $3 for compensation. Six participants did not complete at least 80% of the items and were removed from the study. Thus, the effective sample size was 294. Demographics are presented in the Results section.
Materials and procedures
Participants took an online survey developed by Qualtrics. Our study did not set a specific time restriction. Across 294 participants, the average survey completion time was 682.8 s (SD = 286.6 s). The median completion time was 595.0 s (IQR = 344.8 s). The following questionnaires were completed.
Attitudes toward abortion
Hoffmann and Johnson ( 2005 ) and Osborne et al. ( 2022 ) analyzed attitudes toward abortion with six different scenarios (scenarios a-f below) that were measured by the U.S. General Social Survey. We further added an additional item regarding underage pregnancy for two reasons. First, compared to other Western industrialized nations, the U.S. has historically had a higher rate of underage pregnancies. Additionally, underage pregnant individuals tended to have a higher likelihood of seeking abortions compared to their older counterparts (Lantos et al., 2022 ; Kearney and Levine, 2012 ; Sedgh et al., 2015 ). Second, underage pregnancy is linked to various adverse outcomes, such as increased risk during childbirth, heightened stress and depression, disruptions in education, and financial challenges (Eliner et al., 2022 ; Hodgkinson et al., 2014 ; Kearney and Levine, 2012 ). Given the significance and prevalence of underage pregnancy, we chose to include it as a scenario to understand the public’s perception. Additionally, we understood that people might feel conflict or uncertain toward one or more scenarios. Hence, instead of using binary response (yes/no format) adopted in the U.S. General Social Survey, we employed a 1 to 7 Likert scale for each scenario, with a higher score indicating stronger support for a pregnant woman to obtain legal abortion.
The seven scenarios in the present study included: (a) there is a strong chance of serious defect in the baby; (b) the woman’s own health is seriously endangered by the pregnancy; (c) the woman became pregnant as a result of rape; (d) the woman is married and does not want any more children; (e) the family has a very low income and cannot afford any more children; (f) the woman is not married and does not want to marry the man; and (g) the woman is underage.
Following the wording used to measure empathy in Pfattheicher et al. ( 2020 ), we developed six items to measure the empathy toward the pregnant woman and unborn or fetus, respectively. The scale of empathy toward pregnant woman included: (a) I am very concerned about the pregnant woman who may lose access to legal abortion; (b) I feel compassion for the pregnant women who may lose access to legal abortion; and (c) I am quite moved by the pregnant women who may lose access to legal abortion. The scale of empathy toward unborn included: (a) I am very concerned about the fetus or unborn child; (b) I feel compassion for the fetus or unborn child; and (c) I am quite moved by the fetus or unborn child. Participants rated each item on a five-point Likert scale, with 1 being strongly disagree and 5 being strongly agree. Thus, a higher score demonstrated stronger empathy toward the target. The Cronbach’s α for the scale of toward pregnant woman was 0.90 in the present study. The Cronbach’s α for the scale of toward unborn was 0.92.
The need for cognition scale (NFC, Cacioppo et al., 1984 ) intends to measure the tendency to engage into deep thinking. It has 18 items, such as “I only think as hard as I have to” and “I find satisfaction in deliberating hard and for long hours”. Participants rated each item on a five-point Likert scale, with a higher score indicating a greater tendency to enjoy deep thinking. In the present study, the reliability of this scale was 0.93.
The present study adopted Levenson multidimensional locus of control scale (Levenson, 1981 ). Across 24 items, this scale measures three dimensions of locus of control: internality (sample item: Whether or not I get to be a leader depends mostly on my ability); powerful others (sample item: I feel like what happens in my life is mostly determined by powerful people); and chance (sample item: To a great extent my life is controlled by accidental happenings). In the present study, participants rated each item on a 1 to 6 Likert scale, with a higher score indicating a stronger belief that fate was controlled by self, powerful others, or chance. The Cronbach’s α for the subscales of internality, powerful others, and chance was 0.84, 0.91, and 0.93, respectively. As shown below, there was a high agreement between powerful others and chance subscales ( r = 0.87, p < 0.001). Hence, we combined these two subscales to form an external locus of control composite.
Demographics
After completing the scales described above, participants were asked to report their demographic information including race, age, gender, education, annual household income, current relationship status, abortion experience, religious belief, and political ideology. Gender was coded with 1 = male, 2 = female, and 3 = other. Race was coded with 1 = White or Caucasian, 2 = Hispanic or Latinx, 3 = Black or African American, 4 = Asian or Asian American, and 5 = Other. Education was coded with six levels: 1 = Less than high school graduate, 2 = High school graduate or equivalent, 3 = Some college or associate degree, 4 = Bachelor’s degree, 5 = Master’s degree, 6 = Doctoral degree. Annual household income was categorized into 13 levels and ranged between under $9,999 and above $120,000 with increments of $9,999. Current relationship status was coded into six levels: 1 = single and not dating, 2 = single but in a relationship, 3 = married, 4 = divorced, 5 = widowed, 6 = other. For abortion experience participants were asked “For any reason, have you had an abortion?”. For this question, the answer was coded with 1 = yes and 2 = no.
Religious belief was measured with three items. The first item asked “How often do you attend religious services?” Participants selected one option out of the following: 1 = never, 2 = a few times per year, 3 = once a month, 4 = 2–3 times a month, 5 = once a week or more. The second item asked “How important is religion to you personally?” Participants rated this question on a five-point Likert point, with 5 being most important. The third question asked “How would you describe your religious denomination”. The options included 1 = Christian, 2 = Islam, 3 = Judaism, 4 = Buddhism, 5 = Hinduism, 6 = other or atheism. In the present study, the first two items were highly correlated ( r = 0.77, p < 0.001). Following Hunt ( 2019 ), we combined the two items to form a general religiosity composite, with a higher score indicating a stronger religious belief.
Political ideology was measured with two items: (a) Generally, how would you describe your views on most social political issues (e.g., education, religious freedom, death penalty, gender issues, etc.)? and (b) Generally, how would you describe your views on most economic political issues (e.g., minimum wage, taxes, welfare programs, etc.)? Participants rated each item with a five-point Likert scale, with 1 = strongly conservative 2 = conservative 3 = moderate 4 = liberal 5 = strongly liberal. We found a strong correlation between the two political ideology items, r = 0.76, p < 0.001. Hence, we combined the two items to form a general political ideology composite.
SPSS 24.0 was employed to perform all the analyses. Across 294 participants, age ranged from 21 to 79, with a mean of 40.4 and a standard deviation of 12.4. Table 1 displays the descriptive statistics for the variables of gender, race, education, annual household income, current relationship status, religious denomination, and abortion experience.
Table 2 presents the descriptive statistics of attitudes toward abortion in different scenarios, religious belief, political ideology, and the scores of the psychological scales. Similar to the results obtained from the large-scale surveys in the U.S. and New Zealand (Osborne et al., 2022 ), the support toward abortion was strong (neutral = 4) across all scenarios.
To examine the structure of attitudes toward abortion in different scenarios, a Principal Component Analysis (PCA) with a Varimax orthogonal rotation was performed on all seven scenarios. With eigenvalue ≥ 1 as the threshold, two components were generated, accounting for 81.34% of the variability. Table 3 presents the PCA results. As shown, we obtained two distinct components. The first one included the scenarios of baby defection, pregnant woman’s health being endangered, pregnancy caused by rape, and underage pregnancy. The second component included the scenarios of not wanting the child, low income, and not wanting to marry. Such a differentiation between the two components was consistent with the notion in Osborne et al. ( 2022 ). Following this paper and the face validity of the scenarios, we labeled the two components traumatic abortion and elective abortion, respectively. Accordingly, we also computed a composite score for each component by averaging the corresponding items. In line with previous research (Hoffmann and Johnson, 2005 ), the support was significantly stronger toward the traumatic abortion (mean = 5.84, SD = 1.24) than the elective abortion (mean = 4.94, SD = 1.74), t (293) = 11.51, p < 0.001, Cohen’s d = 0.67.
Table 4 presents the zero-order correlations between attitudes toward traumatic and elective abortions, demographics, and scores of the psychological factors. Consistent with the findings from past research (e.g., Hess and Rueb, 2005 ; Holman et al., 2020 ), a stronger religious belief was negatively related to the support toward both types of abortions. A stronger liberal ideology was positively related to the support toward both types of abortions. Additionally, empathy toward the pregnant woman was positively associated with the support toward both types of abortions whereas empathy toward unborn or fetus had an opposite effect. Based on the zero-order correlation, we did not find a significant relationship between internal locus of control and attitudes toward either type of abortion. The external locus of control (either powerful others or chance), on the other hand, was positively related to the support toward elective but not traumatic abortion. As there was a high agreement between the two external locus of control subscales ( r = 0.87, p < 0.001), we formed a general external locus of control composite by averaging the two items in the following regressions. Finally, need for cognition was positively related to attitudes toward elective abortion but not traumatic abortion.
While the zero-order correlations were informative, we were mindful that the Type I error might be greatly inflated due to a vast amount of repeated testing. Moreover, one goal of the study was to examine the role of psychological factors in the presence of religious belief and political ideology. Thus, we performed a hierarchical linear regression on each type of abortion, with age, gender, income, and education in the first block, religious belief and political ideology in the second block, and psychological factors in the third block. We separated the regression between the two types of abortion because the role of predictors might vary. This approach was also employed in Osborne et al. ( 2022 ). Table 5 exhibits the regression results.
As shown in Table 5 , the demographic variables of age, gender, education, and income did not account for a significant portion of the variability in attitudes toward either type of abortion. The present study added to the literature that there might not necessarily be a difference in attitudes toward abortion between males and females (Bilewicz et al., 2017 ; Jelen and Wilcox, 1997 ). By contrast, in the second block, religious belief and political ideology collectively explained a sizable portion of the variability in attitudes toward both types of abortion. In block 3, in the presence of demographic variables including religious belief and political ideology, psychological factors could still account for a significant portion of the variability.
Looking at the individual psychological predictors (for more detailed interpretations please refer to the discussion part), consistent with our hypothesis, empathy toward the pregnant woman was positively associated with the support toward both types of abortion. By contrast, empathy toward the unborn or fetus was negatively associated the support toward abortion. For the factor of locus of control, the internal locus of control was not related to any type of abortion attitudes when zero-order correlation was used (Table 4 ); yet it was positively related to abortion attitudes after all other predictors were taken into account, indicating a suppressing effect. Upon further examination, we identified two suppressors: religious belief and empathy toward the unborn. After removing these two variables, internal locus of control was no longer significant. The observed pattern reflected our previous prediction, indicating that the role of internal locus of control could be complicated by religious beliefs. External locus of control, on the other hand, was positively correlated with the support toward elective abortion. Similarly, need for cognition (NFC) also had a positive relationship with the support toward elective abortion. Neither external locus of control nor NFC had a significant correlation with attituded toward traumatic abortion. Hence, our hypotheses regarding external locus of control and NFC were partially supported. We detailed out interpretation and discussion of the results below.
The present study aimed to provide empirical evidence for the correlations between psychological factors and attitudes toward abortion. As introduced earlier, while it is common to find the involvement of psychology in everyday life attitudes and preferences, attitudes toward abortion are unique and drastically different. Given its unique nature, it lacks empirical evidence regarding whether psychological factors that interplay with attitudes in other areas still apply and, if so, in what capacity they do so. Past research has primarily focused on the role of religious belief and political ideology. Our study demonstrated a substantial involvement ( R 2 change = 0.27 and 0.24 for traumatic and elective abortion, respectively) of the psychological factors, after controlling for religious belief and political ideology. More importantly, these effects were comparable to the variability accounted for by religious belief and political ideology combined, particularly in the elective abortion category. The results highlighted the influential role of psychological factors in shaping attitudes toward abortion.
Additionally, past research has shown the interconnection between psychology and the public’s attitudes toward major societal events. For example, during the Covid-19 pandemic, while the perception of mask-wearing and/or social distancing was highly politicized, studies found that attitudes toward these preventative measures to be related to thinking style, self-control, numeracy, and working memory capacity (Steffen and Cheng, 2023 ; Xie et al., 2020 ; Xu and Cheng, 2021 ). In line with this, our study further underscored the significant influence of psychology on another pressing societal topic: abortion. In the sections below, we detail our findings and relevant implications. We are fully aware that our study was preliminary and hope it could serve as a starting point for future research and practice. We also acknowledge the limitations of our study and address them at the end.
Some past studies on empathy and abortion only considered the empathy toward the pregnant woman (e.g., Brown et al., 2022 ; Homaifar et al., 2017 ; Hunt, 2019 ; Whitaker et al., 2015 ). The present study identified two types of empathy when dealing abortion: empathy toward the pregnant woman and empathy toward the unborn. In the presence of each other, we found that greater empathy toward the pregnant woman was associated with more support toward abortion, whereas greater empathy toward the unborn or fetus was associated with less support toward abortion. Such a pattern suggested that empathy might be a source of conflict feeling. That is, when considering abortion, concerns and care toward pregnant woman and unborn could coexist, potentially leading to conflict and dilemma when people thought about abortion. While the present study examined the public’s attitudes toward abortion with a diverse sample, pregnant women might have a similar pattern of empathy and hence feel conflict and dilemma when thinking about abortion. To cope with such a conflict, it might be beneficial for a counselor to acknowledge conflicting emotions that arise from empathizing with both the unborn and the pregnant individual. Moreover, the counselor could guide the client through the process of reconciling these emotions to alleviate feelings of isolation or confusion the client may experience. Future research in the realms of mental health and counseling should consider integrating these dual empathy perspectives and empirically assess the efficacy of such therapeutic interventions.
Additionally, Hunt ( 2019 ) did not find a significant influence of empathy on abortion attitudes change when participants were exposed to testimonial videos featuring pregnant women discussing the legal obstacles they faced. The disparity between Hunt’s ( 2019 ) findings and our own could potentially be attributed to the inherent stability and longstanding nature of abortion attitudes. Research has found that people’s views on abortion tends to be stable over time (Jelen and Wilcox, 2003 ; Pew Research Center, 2022 ). As a result, it is possible that pre-existing empathy, rather than empathy induced temporarily, was the factor correlated with individuals’ perception and consideration of abortion. Our findings were consistent with this possibility. Together, our findings supported H1a to H1c. Moreover, our study shed more light on empathy by showing its association with distinct views on abortion. The results suggest that future research could investigate how different types of empathy are formed and how they influence the shaping and persuasion of abortion attitudes.
Through qualitative interviews, Sundstrom et al. ( 2018 ) unveiled individual differences in the locus of control when discussing opinions on abortion. However, these interviews might not have fully captured the interplay between internal and external locus of control and other factors involved attitudes toward abortion. To fill the gap, our study employed a quantitative approach to delve deeper into how locus of control correlated with abortion attitudes. Consistent with Levenson ( 1981 ) and Reknes et al. ( 2019 ), we found that the constructs internal locus of control and external locus of control were differentiated but not unidimensional. For internal locus of control, interestingly, we found a suppressing effect. As discussed earlier, the role of internal locus of control in abortion attitudes might be complicated. That is, on the one hand, by face validity, the internal locus of control well aligned with the concept of “my body, my choice” (Sundstrom et al., 2018 ). On the other hand, in line with past research (Coursey et al., 2013 ; Falkowski, 2000 ; Iles-Caven et al., 2020 ), our study found that internal locus of control was positively related to religious belief. Furthermore, as shown in Table 4 , internal locus of control was also positively related to the empathy toward the unborn, and such a relationship was significantly mediated by religious belief (mediation effect = 0.21, SE = 0.5, 95% CI = [0.13, 0.31]). Therefore, when using zero-order correlation, the effect of internal locus of control might be neutralized by the two opposite parts (“my body, my choice” vs. religious belief) discussed above. By contrast, in regression, the “my body, my choice” part stood out because the religiosity part was partialled out by the variables of religious belief and empathy toward the unborn.
In addition to internal locus of control, we also discovered that external locus of control was involved in abortion attitudes. Specifically, we found a positive relationship between external locus of control and support toward elective abortion (H2 was partially supported). Past research has found that locus of control is related to attribution (Falkowski, 2000 ; Reknes et al., 2019 ). Thus, our finding was in line with the notion that those with a greater level of external locus of control might be more likely to attribute unwanted pregnancy to external reasons (not personal responsibility), and hence showed more support toward abortion.
Our findings regarding locus of control suggest that individuals might simultaneously believe in personal autonomy (“my body, my choice”) while also feeling that certain life events, like unwanted pregnancies, are influenced by external factors beyond their control. This is particularly true when thinking about elective abortion. Education and counseling practices might be designed to reflect this duality. For example, materials and discussions could simultaneously emphasize the importance of personal choices and responsibilities, while also exploring societal, cultural, or circumstantial factors that might influence abortion decision. Incorporating both perspectives would allow to create a supportive environment where individuals feel seen and acknowledged in their complexities.
As introduced earlier, past research on the relationship between thinking style and abortion attitudes was inconclusive. To clarify the relationship, the present study adopted the validated need for cognition scale. Need for cognition has demonstrated its involvement in consequential events, such as political elections and the adoption of preventive measures during the Covid-19 pandemic (Sohlberg, 2019 ; Xu and Cheng, 2021 ). In the present study, we discovered that need for cognition was positively related to the support toward elective abortion. Such a finding was consistent with the notion that need for cognition was negatively related to stereotypes (Crawford and Skowronski, 1998 ; Curşeu and de Jong, 2017 ). Additionally, as need for cognition drives individuals to seek and update knowledge, our result was also in line with the finding that gaining knowledge about abortion led to more positive view on abortion (Hunt, 2019 ; Mollen et al., 2018 ). Our study implied that future research could empirically evaluate if indeed abortion knowledge mediates the relationship between need for cognition and abortion attitudes.
It is worth noting that the present study also clarified the role of need for cognition in attitudes toward abortion by examining a potential artifact. Specifically, the observed positive relationship between need for cognition and support for abortion might be an artifact, given that liberal ideology is positively correlated with both abortion attitudes and need for cognition (Young et al., 2019 ). However, as shown in our regression, the relationship between need for cognition and elective abortion remained significant in the presence of other variables, including political ideology. Thus, the finding suggested that at least part of the relationship between need for cognition and attitude toward abortion was unique and not driven by political ideology.
Our findings related to need for cognition had an implication on abortion-related education. As discussed earlier, having adequate knowledge about abortion could facilitate the support for making informed decisions. As need for cognition was found to be related to openness and motivation to seek and update information (Russo et al., 2022 ), our finding suggested that cultivating willingness to engage into critical thinking might be beneficial for education on abortion and reproductive rights. While we are fully aware that correlation does not equate to causation, our study still offers a starting point for future research and practice on abortion-related education.
Traumatic abortion vs. elective abortion
While some researchers argued that the dichotomization of “pro-choice” and “pro-life” was oversimplified, to date, only two studies have empirically examined attitude variation between different abortion scenarios (Hoffmann and Johnson, 2005 ; Osborne et al., 2022 ). Both studies demonstrated that public views on abortion can be grouped into two categories: traumatic and elective. Our research not only replicated these findings but also introduced two significant advancements. First, we incorporated a scenario addressing underage pregnancy, given its high prevalence and significance. Secondly, instead of a binary response, we employed a 7-point Likert scale, allowing us to more accurately capture potential conflicting attitudes among participants.
Furthermore, our findings revealed that the roles of external locus of control and need for cognition varied in relation to attitudes toward the two types of abortion. Interestingly, we observed that neither of these variables significantly related to attitudes toward traumatic abortion, as indicated by both zero-order correlation and regression analyses. Conceptually, the scenarios of traumatic abortion (e.g., pregnancy caused by rape; mother life endangered) tend to be more extreme and emergent than the scenarios of elective abortion. Hence, there might be less room for psychological factors, such as thinking or attribution, to function in traumatic abortion than in elective abortion. Our interpretation was also consistent with the statistical pattern between the two abortions. That is, compared to elective abortion, the standard deviation of traumatic abortion was smaller. Additionally, there were more participants rated seven on the Likert scale in the scenarios of traumatic abortion (29.6%) than in the scenarios of elective abortion (18%). Despite the difference between the two types of abortion, it is essential to acknowledge that elective abortion does not imply a stress-free experience. Both traumatic and elective abortions involve significant levels of stress and emotional challenges. While traumatic abortion scenarios can be considered more extreme, it is crucial to recognize that individuals undergoing elective abortion may also experience considerable emotional distress.
Taken together, with concrete evidence, our study demonstrated that the public’s attitude toward abortion depended on abortion reasons. Our study also implied that future research should focus on attitudes toward specific abortion scenarios rather than a holistic concept of abortion. Furthermore, the differentiation between the traumatic and elective abortions suggested the limitation and potential ineffectiveness of one-size-fits-all legislative solutions. Given the varying and often conflicting attitudes that people harbor, it would be reasonable for legislative frameworks to be flexible, adaptive, and cognizant of the different circumstances surrounding abortion. This will not only be more reflective of public opinions but also more supportive of individuals who undergo different types of abortion experiences, each of which carries its own set of emotional and psychological challenges.
Expanding findings with a quantitative approach
Some past studies employed a qualitive approach when dealing with attitudes toward abortion (e.g., Dozier et al., 2020 ; Sundstrom et al., 2018 ; Valdez et al., 2022 ; Woodruff et al., 2018 ). These investigations have provided insights and served as inspirations for our own research. However, the relationship between abortion attitudes and pertinent factors may remain somewhat opaque. This is particularly true when considering the intricate interconnectedness among these factors. The present study demonstrated that findings from qualitative studies could be extended and enriched with a quantitative approach. For instance, we utilized quantitative scales to measure empathy toward the unborn —a variable that was previously identified through interviews in the study by Dozier et al. ( 2020 ). Moreover, we further exhibited the role of empathy toward the unborn when statistically controlled other variables, including empathy toward the pregnant. Similarly, the role of internal locus of control was revealed in interviews in Sundstrom et al. ( 2018 ). With validated scales, we exhibited the correlation with internal locus of control in both types of abortion. Furthermore, by detecting and interpreting a suppressing effect, we showed the interplay between internal locus of control, religious belief, and attitude toward abortion. Thus, our study implied that using quantitative scales and analyses was a viable approach to examine attitude toward abortion and could deepen the understanding of relevant factors.
Limitations and future directions
Despite the contributions, limitations should be acknowledged as well. First and foremost, we believe our study was still in the explorative stage. The specific psychological factors tested in the present study were not exhaustive and not theoretically driven. We hope the present study could provide initial empirical evidence to show the sophisticated role of psychology in attitudes toward abortion. Future studies could use a more theoretical driven approach to examine the specific psychological involvement in abortion attitudes. For example, given the correlation between need for cognition and attitudes toward abortion, future research could further elucidate the role of thinking style in attitudes toward abortion by incorporating the Dual-Process Theory (Evans, 2008 ). The Dual-Process Theory posits that humans have two distinct systems of information processing: System 1, which is intuitive, automatic, and fast; and System 2, which is deliberate, analytical, and slower. By examining the interplay between these two systems, researchers might gain insights into how intuitive emotional responses versus more deliberate cognitive analyses influence individuals’ attitudes toward abortion. For instance, are individuals who predominantly rely on System 1 more swayed by emotive narratives or imagery related to abortion?
Second, when analyzing and discussing the results, we proposed several possible underlying mechanisms that might elucidate the relationships observed. To illustrate, we employed the concept of attribution to shed light on the role of an external locus of control, positing that individuals with a strong external locus might attribute abortion decisions to external factors or circumstances rather than personal choices. Furthermore, we suggested that the observed positive relationship between the need for cognition and abortion attitudes might be mediated through abortion knowledge. This implies that individuals with a higher need for cognition could potentially seek out more information on abortion, leading to more informed attitudes. However, while these interpretations offer potential insights, we recognize their speculative nature. It’s crucial to emphasize that our proposed mechanisms require rigorous empirical testing for validation. For example, it would be of interest to test whether indeed, gaining various types of abortion knowledge improves views of abortion.
Third, as described above, we strived to show how our findings could be potentially used in abortion-related counseling. However, we acknowledge that our study is explorative but not counseling focused. Therefore, while we believe our findings offer meaningful implications, we caution against over-extrapolating their direct applicability to counseling contexts. Future research could delve into empirically investigating how psychological factors, such as varying empathy types and loci of control, could be utilized to alleviate negative feelings associated with abortion decisions. Additionally, understanding how various psychological factors interact with cultural and social norms could further help tailor counseling approaches.
Fourth, the present study did not include an attention check item. We believe the quality of our survey could have been improved had we included one or more attention check items. However, the reliabilities of our scales were relatively high (ranged from 0.84 to 0.93). Additionally, we also replicated some major findings from previous research (e.g., the associations between attitudes toward abortion and religious belief and political ideology). Thus, we believe that overall, inattention did not affect the quality of our data. Future online surveys could consider using attention check items for quality control.
In conclusion, the present study demonstrates the unique contribution of empathy, locus of control, and need for cognition to how people perceived abortion in different scenarios. The findings suggests that attitudes toward complex moral issues like abortion are shaped by individual psychological traits and cognitive needs, in addition to societal, religious, and cultural norms. Future research could use our study as a starting point to expand on these findings, exploring other psychological traits and cognitive processes that may similarly affect perceptions of abortion and other controversial subjects.
Data availability
Data included in this project may be found in the online repository, https://doi.org/10.7910/DVN/E5AB5R .
Batson CD, Polycarpou MP, Harmon-Jones E, Imhoff HI, Mitchener EC, Highberger L et al. (1997) Empathy and attitudes: can feeling for a member of a stigmatized group improve feelings toward the group? J Person Soc Psychol 72(1):105–118
Article CAS Google Scholar
Bilewicz M, Mikołajczak G, Babińska M (2017) Speaking about the preborn. How specific terms used in the abortion debate reflect attitudes and (de)mentalization. Person Individ Differ 111:256–262
Article Google Scholar
Brown L, Swiezy S, McKinzie A, Komanapalli S, Bernard C (2022) Evaluation of family planning and abortion education in preclinical curriculum at a large midwestern medical school. Heliyon 8(7):e09894. https://doi.org/10.1016/j.heliyon.2022.e09894
Article PubMed PubMed Central Google Scholar
Cacioppo JT, Petty RE, Kao CF (1984) The efficient assessment of need for cognition. J Person Assess 48(3):306–307. https://doi.org/10.1207/s15327752jpa4803_13
Comrey AL, Lee HB (1992) A first course in factor analysis (2nd ed.). Lawrence Erlbaum Associates, Inc
Coursey LE, Kenworthy JB, Jones JR (2013) A meta-analysis of the relationship between intrinsic religiosity and locus of control. Arch Psychol Relig 35:347–368. https://doi.org/10.1163/15736121-12341268
Crawford MT, Skowronski JJ (1998) When motivated thought leads to heightened bias: high need for cognition can enhance the impact of stereotypes on memory. Person Soc Psycholo Bull 24(10):1075–1088. https://doi.org/10.1177/01461672982410005
Curşeu PL, de Jong JP (2017) Bridging social circles: need for cognition, prejudicial judgments, and personal social network characteristics. Front Psychol 8:1251. https://doi.org/10.3389/fpsyg.2017.01251
Ding D, Chen Y, Lai J, Chen X, Han M, Zhang X (2020) Belief bias effect in older adults: roles of working memory and need for cognition. Front Psychol 10:2940. https://doi.org/10.3389/fpsyg.2019.02940
Dozier JL, Hennink M, Mosley E, Narasimhan S, Pringle J, Clarke L, Blevins J, James-Portis L, Keithan R, Hall KS, Rice WS (2020) Abortion attitudes, religious and moral beliefs, and pastoral care among Protestant religious leaders in Georgia. PloS one 15(7):e0235971. https://doi.org/10.1371/journal.pone.0235971
Article CAS PubMed PubMed Central Google Scholar
Eliner Y, Gulersen M, Kasar A, Lenchner E, Grünebaum A, Chervenak FA, Bornstein E (2022) Maternal and neonatal complications in teen pregnancies: a comprehensive study of 661,062 patients. J Adolesc Health 70(6):922–927. https://doi.org/10.1016/j.jadohealth.2021.12.014
Article PubMed Google Scholar
Embree RA (1998) Attitudes toward elective abortion: preliminary evidence of validity for the personal beliefs scale. Psychol Rep 82(3 Pt 2):1267–1281. https://doi.org/10.2466/pr0.1998.82.3c.1267
Article CAS PubMed Google Scholar
Evans JSTBT (2008) Dual-processing accounts of reasoning, judgment and social cognition. Ann Rev Psychol 59:255–278. https://doi.org/10.1146/annurev.psych.59.103006.093629
Falkowski CK (2000) Locus of control, religious values, work values and social policy choices. Diss Abstracts Int. Sec B: Sci Eng 61:1694
Google Scholar
Felix., M., Sobel, L., & Salganicoff, A. (2023). Legal challenges to state abortion bans since the dobbs decision. Kaiser Family Foundation . Retrieved from https://www.kff.org/womens-health-policy/issue-brief/legal-challenges-to-state-abortion-bans-since-the-dobbs-decision/
Fischhoff B, Broomell SB (2020) Judgment and decision making. Ann Rev Psychol 71:331–355
Foster DG, Gould H, Taylor J, Weitz TA (2012) Attitudes and decision making among women seeking abortions at one U.S. clinic. Perspect Sexual Reprod Health 44(2):117–124. https://doi.org/10.1363/4411712
Hess JA, Rueb JD (2005) Attitudes toward abortion, religion, and party affiliation among college students. Curr Psychol 24(1):24–42. https://doi.org/10.1007/s12144-005-1002-0
Hill A (2004) The relationship between attitudes about abortion and cognitive complexity. UW-J Undergrad Res VII:1–6
ADS Google Scholar
Hodgkinson S, Beers L, Southammakosane C, Lewin A (2014) Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics 133(1):114–122. https://doi.org/10.1542/peds.2013-0927
Hoffmann JP, Johnson SM (2005) Attitudes toward abortion among religious traditions in the United States: change or continuity. Soc Relig 66(2):161–182. https://doi.org/10.2307/4153084
Holman M, Podrazik E, Silber Mohamed H (2020) Choosing choice: how gender and religiosity shape abortion attitudes among Latinos. J Race Ethnicity Politics 5(2):384–411. https://doi.org/10.1017/%20rep.2019.51
Homaifar N, Freedman L, French V (2017) “She’s on her own”: a thematic analysis of clinicians’ comments on abortion referral. Contraception 95(5):470–476. https://doi.org/10.1016/j.contraception.2017.01.007
Hunt ME (2019) Shifting Abortion Attitudes using an Empathy-based Media Intervention: a randomized controlled study. graduate theses and dissertations Retrieved from https://scholarworks.uark.edu/etd/3256
Jelen TG (2017) Public attitudes toward abortion and LGBTQ issues: a dynamic analysis of region and partisanship. SAGE Open 7(1):1–6. https://doi.org/10.1177/2158244017697362
Jelen TG, Wilcox C (1997) Attitudes toward abortion in Poland and the United States. Soc Sci Q 78(4):907–921
Jelen TG, Wilcox C (2003) Causes and consequences of public attitudes toward abortion: a review and research agenda. Political Res Q 56(4):489–500. https://doi.org/10.2307/3219809
Kearney MS, Levine PB (2012) Why is the teen birth rate in the United States so high and why does it matter. J Econ Perspect 26(2):141–166. https://doi.org/10.1257/jep.26.2.141
Kim-Prieto C, Diener E, Tamir M, Scollon C, Diener M (2005) Integrating the diverse definitions of happiness: a time-sequential framework of subjective well-being. J Happiness Studies 6(3):261–300. https://doi.org/10.1007/s10902-005-7226-8
Klimecki O, Mayer S, Jusyte A et al. (2016) Empathy promotes altruistic behavior in economic interactions. Sci Rep 6:31961. https://doi.org/10.1038/srep31961
Article ADS CAS PubMed PubMed Central Google Scholar
Klimecki OM (2019) The role of empathy and compassion in conflict resolution. Emotion Rev 11(4):310–325
Krause N, Hayward RD (2013) Prayer beliefs and change in life satisfaction over time. J Relig Health 52:674–694
Lantos, H., Pliskin, E., Wildsmith, E., & Manlove, J. (2022). State-level abortion restrictions will negatively impact teens and children. Child Trend s. Retrieved from https://www.childtrends.org/blog/state-level-abortion-restrictions-will-negatively-impact-teens-and-children
Levenson H (1981) Differentiating among internality, powerful others, and chance. In: Lefcourt HM (Ed.) Research with the Locus of Control Construct. Academic Press, New York, NY, p 15–63. 10.1016/b978-0-12-443201-7.50006-3
Iles-Caven Y, Gregory S, Ellis G, Golding J, Nowicki S (2020) The relationship between locus of control and religious behavior and beliefs in a large population of parents: an observational study. Front Psychol 11:1462. https://doi.org/10.3389/fpsyg.2020.01462
Marton G, Pizzoli SFM, Vergani L, Mazzocco K, Monzani D, Bailo L, Pancani L, Pravettoni G (2021) Patients’ health locus of control and preferences about the role that they want to play in the medical decision-making process. Psychol Health Med 26(2):260–266. https://doi.org/10.1080/13548506.2020.1748211
Mollen D, Hargons C, Klann EM, Mosley DV (2018) Abortion knowledge and attitudes among psychologists and graduate students. Counseling Psychol 46(6):738–760. https://doi.org/10.1177/0011000018795296
Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S (2020) The role of empathy in health and social care professionals. Healthcare 8(1):26. https://doi.org/10.3390/healthcare8010026
Osborne D, Huang Y, Overall NC, Sutton RM, Petterson A, Douglas KM, Davies PG, Sibley CG (2022) Abortion attitudes: an overview of demographic and ideological differences. Political Psychol 43:29–76. https://doi.org/10.1111/pops.12803
Pew Research Center. (2022, May 17). Public Opinion on Abortion. Retrieved from https://www.pewresearch.org/religion/fact-sheet/public-opinion-on-abortion/
Pfattheicher S, Nockur L, Böhm R, Sassenrath C, Petersen MB (2020) The emotional path to action: empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol Sci 31(11):1363–1373. https://doi.org/10.1177/0956797620964422
Prusaczyk E, Hodson G (2018) Left-right differences in abortion policy support in America: clarifying the role of sex and sexism in a nationally representative 2016 sample. Person Individual Differ 127:22–25. https://doi.org/10.1016/j.paid.2018.01.030
Reknes I, Visockaite G, Liefooghe A, Lovakov A, Einarsen SV (2019) Locus of control moderates the relationship between exposure to bullying behaviors and psychological strain. Front Psychol 10:446169. https://doi.org/10.3389/fpsyg.2019.01323
Richardson M, Abraham C, Bond R (2012) Psychological correlates of university students’ academic performance: a systematic review and meta-analysis. Psychol Bull 138(2):353–387. https://doi.org/10.1037/a0026838
Russo D, Masegosa AR, Stol KJ (2022) From anecdote to evidence: the relationship between personality and need for cognition of developers. Empir Software Eng 27:71. https://doi.org/10.1007/s10664-021-10106-1
Rye BJ, Underhill A (2020) Pro-choice and pro-life are not enough: an investigation of abortion attitudes as a function of abortion prototypes. Sexuality Culture 24:1829–1851. https://doi.org/10.1007/s12119-020-09723-7
Saad, L. (2023, June 21). Abortion remains a potent issue for pro-choice voters. Gallup . Retrieved from https://news.gallup.com/poll/507527/abortion-remains-potent-issue-pro-choice-voters.aspx
Sedgh G, Finer LB, Bankole A, Eilers MA, Singh S (2015) Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. J Adolesc Health 56(2):223–30
Scott J (1989) Conflicting beliefs about abortion: legal approval and moral doubts. Soc Psychol Q 52(4):319–326. https://doi.org/10.2307/2786995
Shafir E, LeBoeuf RA (2002) Rationality. Ann Rev Psychol 53(1):491–517. https://doi.org/10.1146/annurev.psych.53.100901.135213
Sohlberg J (2019) Elections are (not) exciting: need for cognition and electoral behaviour. Scand Political Stud 42(2):138–150. https://doi.org/10.1111/1467-9477.12138
Steffen J, Cheng J (2023) The influence of gain-loss framing and its interaction with political ideology on social distancing and mask wearing compliance during the COVID-19 pandemic. Curr Psychol 42(10):8028–8038. https://doi.org/10.1007/s12144-021-02148-x
Sundstrom B, Szabo C, Dempsey A (2018) “My Body. My Choice”: a qualitative study of the influence of trust and locus of control on postpartum contraceptive choice. J Health Commun 23(2):162–169. https://doi.org/10.1080/10810730.2017.1421728
Valdez D, Jozkowski KN, Haus K et al. (2022) Assessing rigid modes of thinking in self-declared abortion ideology: natural language processing insights from an online pilot qualitative study on abortion attitudes. Pilot Feasib Stud 8:127. https://doi.org/10.1186/s40814-022-01078-0
Verplanken B, Hazenberg PT, Palenéwen GR (1992) Need for cognition and external information search effort. J Res Person 26(2):128–136. https://doi.org/10.1016/0092-6566(92)90049-A
Whitaker AK, Quinn MT, Martins SL, Tomlinson AN, Woodhams EJ, Gilliam M (2015) Motivational interviewing to improve postabortion contraceptive uptake by young women: development and feasibility of a counseling intervention. Contraception 92(4):323–329. https://doi.org/10.1016/j.contraception.2015.06.015
Woodruff K, Biggs MA, Gould H, Foster DG (2018) Attitudes toward abortion after receiving vs. being denied an abortion in the USA. Sexuality Res Soc Policy 15(4):452–463. https://doi.org/10.1007/s13178-018-0325-1
Xie W, Campbell S, Zhang W (2020) Working memory capacity predicts individual differences in social distancing compliance during the COVID-19 pandemic in the U.S. PNAS 117(30):17667–17674
Article ADS PubMed PubMed Central Google Scholar
Xu P, Cheng J (2021) Individual differences in social distancing and mask-wearing in the pandemic of COVID-19: the role of need for cognition, self-control and risk attitude. Person Individual Differ 175:110706. https://doi.org/10.1016/j.paid.2021.110706
Young DG, Bagozzi BE, Goldring A, Poulsen S, Drouin E (2019) Psychology, political ideology, and humor appreciation: why is satire so liberal. Psychol Popular Media Culture 8(2):134–147. https://doi.org/10.1037/ppm0000157
Download references
Author information
Authors and affiliations.
University of Northern Iowa, Cedar Falls, IA, 50614, USA
Jiuqing Cheng & Chloe Thostenson
Wenzhou University, Wenzhou, China
You can also search for this author in PubMed Google Scholar
Contributions
JC: conceptualization, data curation and analysis, writing, review& editing; PX: conceptualization, writing, review; CT: conceptualization, data curation and analysis, review.
Corresponding author
Correspondence to Jiuqing Cheng .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board (IRB 23-0018) at the University of Northern Iowa with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Cheng, J., Xu, P. & Thostenson, C. Psychological traits and public attitudes towards abortion: the role of empathy, locus of control, and need for cognition. Humanit Soc Sci Commun 11 , 23 (2024). https://doi.org/10.1057/s41599-023-02487-z
Download citation
Received : 18 July 2023
Accepted : 30 November 2023
Published : 02 January 2024
DOI : https://doi.org/10.1057/s41599-023-02487-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Abortion Restrictions and the Threat to Women’s Health
The abortion rights landscape a year after Roe v. Wade was overturned
Annalies Winny
It’s been almost a year since the U.S. Supreme Court overturned Roe v. Wade , dismantling the constitutional right to abortion more than 50 years after the case was decided.
Now, the legal battleground of reproductive rights has grown even more tense. At least a dozen states have banned abortion entirely, and more states are seeking to further restrict access to abortion—making the U.S. an outlier on the global stage: Some 59% of the world's female population currently reside in a country where abortion is broadly allowed.
“And generally over the past several decades, there has been a trend toward increasing liberalization. So this is part of a very unique change in policy happening in the U.S.,” Suzanne Bell , PhD ’18, MPH, said during a May 18 media briefing .
During the briefing, Bell, an assistant professor in Population, Family and Reproductive Health at the Bloomberg School, and Joanne Rosen , JD, MA, a senior lecturer in Health Policy and Management , discussed the state of abortion access in the U.S. and the impact on women’s health—and on physicians—since Roe was overturned. They outlined how abortion restrictions worsen health disparities, how states have responded to Roe’s dismantling, and the potential ramifications of litigation to restrict access to medication abortion for women across the country.
How states have responded
With federal protections for abortion overturned, states were empowered to regulate reproductive health. Rosen noted that some have passed legislation shoring up access to abortion. Fifteen states where abortion remains legal have enacted various additional protections, such as permitting the use of state funds to cover abortion costs; allowing non-physician health professionals to perform abortions; protecting physicians from prosecution, extradition, or other legal action by states that have banned abortion; and prohibiting the disclosure of patients’ medical records without patient permission.
Other states, however, have moved to further erode access, Rosen explained. Even before Dobbs was decided, abortion-hostile states enacted 108 abortion restrictions —in 2021 alone. This is the single highest number of abortion restrictions in any year since Roe was decided in 1973, according to the Guttmacher Institute. In the 11 months since Dobbs was decided, abortion has been banned in 14 states.
Efforts to ban medication abortion nationwide
A Texas case seeking to revoke the FDA’s approval of the safe and effective drug mifepristone—which was used in 53% of abortions in 2020—has “extraordinary” implications that go beyond the possibility of taking mifepristone off the shelves, said Rosen. The litigation also sets a dangerous precedent for court interference in the FDA’s scientific approval process. If the plaintiffs are successful, it “would be the first time a court has abrogated the FDA’s approval of a drug over the objections of the FDA,” Rosen explained. The consequences could be far-reaching, potentially affecting access to any number of drugs for political or ideological reasons.
Other efforts to abolish abortion center on reviving the Comstock Act, an 1873 law banning, among other things, the mailing or transport of products “intended for the prevention of conception or procuring of abortion.” The Comstock Act is one of many “zombie laws”—meaning they’ve long been considered invalid but remain technically on the books—that could see a revival given the precedent set by overturning Roe and invalidating Planned Parenthood v. Casey , the 1992 decision that upheld the right to abortion. Other “zombie laws” in the same legal vein as Comstock, with the same potential for revival, concern same sex marriage and sexual activity and interracial marriage.
Concerns for physicians
The wave of abortion bans have broader implications for the health care workforce.
For one, physicians working in states that ban abortion must contend with “risk management committees” set up by hospitals to determine whether an abortion is warranted in an urgent health care situation where the life of a pregnant person is at risk. “In this context, physicians are finding it difficult to use best medical practices to protect their patients’ well-being”—and they’re concerned about the genuine risk of criminal prosecution, Rosen said.
In this environment, it’s getting harder for hospitals in abortion-hostile states to attract and retain obstetricians and gynecologists, and raising questions about the future of training for these specialties in those states.
“Are they going to entirely leave hostile states and set up their training program elsewhere?” asked Bell. “Or are the people that received training in those states just not going to receive the appropriate training? I think we have yet to see what those full ramifications are.”
Deepening disparities
All of these challenges stand to exacerbate existing disparities in access to quality reproductive health care, Bell added.
Black women are three times as likely, and Hispanic women twice as likely, to seek abortions than white women. And half of all women who get abortions live below the poverty line—many of them in states that limit or are seeking to limit abortions, explained Bell .
Being denied an abortion comes with substantial health risks—especially for vulnerable groups. The risk of maternal death is 15 times higher for carrying a pregnancy to term than it is for abortion, and pregnancy-related complications are 2 to more than 25 times higher for pregnancies ending in birth compared to abortion, Bell explained.
“We have maternal mortality rates that are in some cases twice as high in restrictive states as they are in supportive abortion states,” said Bell—and those restrictions undermine the delivery of basic services, Bell added.
“I want to emphasize that abortion is health care,” Bell said. “Recent state restrictions, coupled with ongoing efforts to curtail access to medication abortion pills nationwide, are an attempt to interfere with the delivery of evidence-based health care and control pregnant people’s bodies, with harmful consequences for individuals and population health.”
Annalies Winny is a producer and writer at the Johns Hopkins Bloomberg School of Public Health.
- A Brief History of Abortion in the U.S.
- Mifepristone On Trial: An Unprecedented Overreach (podcast)
- What’s Happening With Abortion Access Six Months After the SCOTUS Decision (podcast)
Related Content
An update on measles, pertussis, mpox, and other vaccine-preventable diseases, post-election public health needs to keep on keeping on, alumni spotlight: rachel milkovich, student spotlight: daisy zapata, student spotlight: annaliese collins.

IMAGES
COMMENTS
Using robust consensus science methods we have developed a core outcome set for future abortion research. Standardized outcomes in abortion research could decrease heterogeneity among trials and improve the quality of systematic reviews and clinical guidelines.
We identify four interrelated facets of the U.S. abortion imaginary pertaining to who gets an abortion and why: maternal inevitability, economic decision-making, relationship precarity, and emotional fragility.
Jung and colleagues review current practice and evidence on medication abortion, procedural abortion, and associated reproductive health care, as well as implications for training environments in...
These pivotal evidence-based recommendations and best practices recognise the needs of pregnant individuals across the abortion care pathway, calling for the removal of unnecessary policy barriers and providing clear guidance to health-care providers for the delivery of safe abortion care.
We defined harm reduction in the context of abortion as the direct provision (by any kind of healthcare provider) of information about safe abortion methods to pregnant persons seeking induced abortion.
The abortion and mental health controversy is driven by two different perspectives regarding how best to interpret accepted facts. When interpreting the data, abortion and mental health proponents are inclined to emphasize risks associated with ...
The authors evaluated empirical research addressing the relationship between induced abortion and women’s men-tal health. Two issues were addressed: (a) the relative risks associated with abortion compared with the risks associ-ated with its alternatives and (b) sources of variability in women’s responses following abortion. This article ...
The legal context for abortion – whether or not the state allows abortions and how it regulates them – sets the framework for providers of abortion services and for the women who seek such services.
Here we propose that examining the correlations between psychological factors and attitudes toward abortion has the potential to make contributions from the perspectives of both research and...
They outlined how abortion restrictions worsen health disparities, how states have responded to Roe’s dismantling, and the potential ramifications of litigation to restrict access to medication abortion for women across the country.