Nursing Case Study for Diabetic Foot Ulcer
Watch More! Unlock the full videos with a FREE trial

Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Michael is a 15-yr-old male diagnosed with type I diabetes mellitus (DM) last year. He presents to the acute care clinic with a “sore that will not heal” on the bottom of his right foot. He states that he sees an endocrinologist for his DM but has no other health issues to report at this time. He also says that he exercises frequently under the guidance of a dietician and personal trainer consulted through endocrinology and still wrestles for his high school team
His mother is with him and gives consent for treatment. She says, “The pad of his foot has not even been hurting him but when he was pushing off the wrestling mat in practice, he noticed something there.”
What does the nurse suspect may be going on with Michael today? Why?
- A diabetic foot ulcer.
- He is at high risk for foot ulcers (“The lifetime risk of a foot ulcer in patients with diabetes [type 1 or 2] may be as high as 34 percent”)
- He seems to have neuropathy because he does not feel the wound
- He says it will not heal (could be due to many factors especially high blood glucose)
- Assessment should include evaluating and documenting the following:
- Size and depth of the wound
- Color of wound (area and base)
- Look for drainage (exudate)
- Check for loss of sensation (pinprick, touch, pressure) in the lower extremities
- Vascular status (pulse, claudication) in the lower extremities
The nurse notices she cannot feel pedal pulses and the feet seem cool, but not cold. However, the area around the wound is warmer and red. Both feet are WNL in regard to color. Michael denies any cramping or pain in his legs.
What should the nurse do now? How would she document this finding?
- She should get a doppler device prior to proceeding. The pulse may only be weak, not absent. Care should be taken not to document “absent pulse” without first attempting a doppler pulse. Documentation should include whether pulses are palpable or doppler only.
The wound has a slightly foul odor and has a circular “punched out” shape almost like a red based crater. Michael’s mother asks how this could happen.
How should the nurse explain Michael’s risks for this condition?
- Foot problems are a common complication in people with diabetes. Poor glucose control can lead to vascular problems (poor circulation), neuropathy, higher risk for infection (impeding white blood cells from doing their job).
- “Risk factors that can lead to foot wounds in patients with diabetes include loss of protective sensation due to neuropathy, prior ulcers or amputations, foot deformity leading to excess pressure, external trauma, infection, and the effects of chronic ischemia, typically due to peripheral artery disease. Patients with diabetes also have an increased risk for non-healing related to mechanical and cytogenetic factors, as well as a high prevalence of peripheral artery disease”
The provider assesses the patient and advises the staff he has put in orders. He also asks for a set of vital signs (which had not yet been taken).
Why would the provider want vital signs when the patient only has a wound on his foot?
- This is a basic part of an assessment and should never be skipped even if the patient seems healthy. If the patient were to have a change, and no vital signs were taken early on, there would be nothing to compare VS to. Also, if he has an infection, his VS could be the first clue if he were to become septic (signs of septic shock).
BP 110/68 SpO2 98% on Room Air HR 92 bpm and regular Pain 0/10 on 1-10 scale with 10 being highest RR 16 bpm at rest Temp 37.9°C
Michael’s mother asks why the acute care clinic cannot just take care of her son’s foot. She says, “Can’t we just get some antibiotics and go?”
How should the nurse address this issue?
- Foot ulcers in diabetics can be complicated to treat. To prevent complications like worsening infection, possible surgery and/or amputation coordinated care is recommended. A culture of the wound may guide the provider’s choice of antibiotic. Especially since Michael does not seem to feel this wound, it should be addressed more carefully than just a “wound.”
Both patient and mother agree to the prescribed treatments. Before they leave, the provider indicates he wants to talk to them about when to seek a higher level of care.
What does the nurse expect the provider to discuss?
- “Management of diabetic foot infections requires attentive wound management, good nutrition, appropriate antimicrobial therapy, glycemic control, and fluid and electrolyte balance. Although severe infections warrant hospitalization for urgent surgical consultation, antimicrobial administration, and medical stabilization, most mild infections and many moderate infections can be managed in the outpatient setting with close follow-up.
- Several studies have reported improved outcomes with a multidisciplinary approach to diabetic foot infections. This includes involvement of specialists in wound care, infectious diseases, endocrinology, and surgery”
What should the nurse ensure she does in regard to discharge teaching?
- If antibiotics are prescribed, whether now or pending wound culture, the full course must be taken even if everything seems to be improving.
- “It is important to examine your feet every day. This should include looking carefully at all parts of your feet, especially the area between the toes. Look for broken skin, ulcers, blisters, areas of increased warmth or redness, or changes in callus formation; let your health care provider know if you notice any of these changes or have any concerns.”
- Take note of any unusual sensations in the feet and legs, including pain, burning, tingling, or numbness. If you notice these symptoms, keep track of when they happen; whether your feet, ankles, and/or calves are affected; and what measures relieve the symptoms.
Michael says he will follow the prescriptions and follow up as instructed. He also wants to know how to keep this from happening again.
What are some tips the nurse can provide regarding prevention? What about resources to provide?
- Avoid smoking
- Avoid going barefoot, even at home, and especially on hot decks and hot sand
- Test water temperature before stepping into a bath
- Trim toenails to the shape of the toe, and remove sharp edges with a nail file; do not cut cuticles
- Wash in lukewarm water, dry thoroughly (including between the toes), and check feet daily
- Shoes should be snug, but not tight, and customized if feet are misshapen or have ulcers
- Socks should fit and be changed daily
- Resources – for this particular patient, he may like audio-visual education resources. There may also be resources available through his endocrinologist’s office.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
References:
View the full transcript, nursing case studies.

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
- High School
- You don't have any recent items yet.
- You don't have any courses yet.
- You don't have any books yet.
- You don't have any Studylists yet.
- Information
Critical Analysis of a Case Study of a Patient with a Diabetic Foot Ulcer
Preparation for professional nursing (nurs 211), prairie state college, recommended for you, students also viewed.
- Diabetic foot ulcer
- Diabetic Study Guide
- Wound and pressure ulcers study guide
- Sociology Lecture Notes Sociology of Culture Unit
- Psych 101 Lecture Notes 10
- Postpartum Complications
Related documents
- NR222 Unit 7
- Pocket Card Management of Upper Gastrointestinal Bleeding January 2023
- Study Guide Part 5 questions answers
- Study Guide Quiz 1 Principles of Therapeutic
- Medication Administration outline study guide.docx
- The Prehospital Therapeutic Hypothermia
Preview text
- Introduction
The current study is a case study analysis aimed at evaluating a patient with a diabetic foot ulcer by providing a discussion on effective care management through the use of systematic care planning. This analysis is essential in the identification of crucial care plans that must be provided systematically to improve the quality of life of the patient and ensure better health management. Additionally, the current analysis will identify how the condition affected the patient physically, socially, and psychologically. As part of the analysis, the research will review relevant health policy, the significance of the support to the patient by health service providers, relevant nursing models, care planning initiatives and other critical elements in the provision of care to diabetic patients with foot ulcers.
- Description of the Condition
Diabetes-associated foot conditions like infections, gangrene, and ulcerations are the common causes of diabetic patients’ hospitalization. According to Kruse and Edelman (2006), routine ulcer care, amputation, treatment of infections, and hospitalization of diabetic patients cost heavily annually and expose the patients to serious health burdens. Mariam, et al (2017) noted that diabetes foot ulcers results in long-term pain and suffering for patients as it is the main cause of complications with a lifetime risk of 25%, despite that most of these occurrences could be avoided. Though the preventive approaches are cost-effective, diabetic foot ulcers
still persist in diabetic patients. The development of the foot ulcer condition is dependent on factors such as age, weight, patient behavior, and lifestyle and the existence of complicated peripheral neuropathy. Snyder and Hanft (2009) state that diabetes foot ulcers result in infections, amputations, and gangrene and sometimes result in death.
- Physical, Sociological, and psychological Impacts
Bahari (2015) noted that though much suffering and pain associated with diabetes foot ulcer is normally physical, the psychological impact of the condition is rarely studied. However, patients with diabetic foot ulcer were reported to experience depression, anxiety, and moments of stress due to the condition. Major depressive disorders accelerate further the negative
care requirements in self-management practices for the patient as well as emotional distress faced by the family.
- Nursing Models and their Significance in Nursing Care Planning
Mattila, et al (2014) explains that nursing models provide the infrastructure that is critical in torganization and delivery of quality care to patients and their families. Additionally, models form the philosophical foundation the patient care and prevailing organizational culture with the increasingly changing needs of individual patients under care. In care practices, nursing models normally affect the number of staff, resource allocation, and organizational cost. Changing nursing roles are affecting nursing models from Nightingale’s care method to relationship-based care
models in primary nursing care (Fairbrother, Jones, & Rivas, 2010). In primary nursing model, the patients care is reflected expressed in terms of responsibility by a named nurse for the entire duration of stay in hospital.
Therefore, planning and implementation of care practices is primarily dependent on the both the named nurse and patient. The named nurse has the responsibility of the patient and is answerable to the patient, collegues and family members. However, this nurse require support from other nurses (Jost, Bonnell, Chacko, & Parkinson, 2010). Understanding primary nursing model facilitates in planning and organisation of care delivery since its grounded on patient- centered approach. Through proper plannnig using the model, a nurse is able to perform the responsibilitys with professionalism, broad job description, autonomy and and independence in decision making (nursing leadership) (Mattila, et al., 2014).
- Clinical Assessment of Diabetic Foot Ulcer
The assessment of the diabetes foot ulcer in the patient was important in determing the severity of the condition in determing the most effective approach depending on its stage. In risk assessment, the nurse conducted assessment of the affected foot. The first assessment form involved focusing on patient’s history of previous amputation or ulceration. Other clinical assessment involved determination of history of impaired vision, peripheral vascular symptoms, renal replacement therapy, tobacco use was recorded smoking habits if any was also recorded. In the OPD when the patient began walking, neuropathy status of the patient was guessed. Due to the ulcer, the patient walked while limping, an indication of possibly a mild to moderate neuropathy. If the patient had moved without a limp, it would be an indication of severe neuropathy. Assessment
After finding the shoe with the patient unfit for the condition, the patient was advised on well fitting shoe to prevent development of blisters. The demartologocal assessment involved the status of affected area of the skin considering regions of abnormal erythema. The assessment nurse also recorded presence or abosence of ingrown toe, nail dystrophy, or paronychia. In addition, the temparature of both feet was evaluated and recorded since the difference could be an indication of celluttis or vascular disease either with or without the ulcer. The tool used in measuring the temparature of both feet was laser thermometer that is considered more precise.
The otther form of assessment conducted involved foot deformities that result to high pressure areas resulting to development of diabetic foot ulceration. Musculoskeletal assessment involved the evaluation of gross foot deformity. The occurrence of rigid deformities involve contractures that is not manually reduced easily and normally found in digits. Presence of forefoot deformities that tend to increase plantar pressures and normally associated with the skin breakdown include hammer or claw toe. Another assessment practice to the patient involved the Charcot arthropathy conditon that is normally misdiagnised or overlooked, which normally occurs in the neuropathic foot affectinog mid foot. It occurs as unilateral red, swollen, hot, flat foot that has profound deformity. Occurrence of rocker-bottom deformity that is secondary to Charcot arthropathy results to excessive pressure in the laner mid-foot that elevates the risk of ulceration on the affected site. If the patient was found developing Charcot arthropathy, she would have been recommended to visit a specialist to conduct further assessment.
- Multiple Choice

Course : Preparation For Professional Nursing (NURS 211)
University : prairie state college.

- Discover more from: Preparation For Professional Nursing NURS 211 Prairie State College 505 Documents Go to course
- More from: Preparation For Professional Nursing NURS 211 Prairie State College 505 Documents Go to course
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

The effectiveness of home-based nursing intervention in the elderly with recurrent diabetic foot ulcers: A case report
Annisa wuri kartika, widyatuti widyatuti, etty rekawati.
- Author information
- Article notes
- Copyright and License information
School of Nursing, Faculty of Medicine, Universitas Brawijaya Malang, Jl Puncak Dieng, Kalisongo, Kecamatan Dau Malang, East Java 65151, Indonesia. Tel. +62.341569117 - +62.341564755. [email protected]
Contributions: All authors contributed equally to this article. AWK conducted this study, WW and ER served as supervisors and reviewed the article.
Conflict of interest: The authors declare that there was no potential conflict of interest.
Conference presentation: Part of this study was presented at the 1 st International Nursing and Health Sciences Symposium, November 13 th to 15 th 2020, Brawijaya University, Malang, Indonesia.
Received 2021 Jan 14; Accepted 2021 Mar 18; Collection date 2021 Apr 15.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License ( http://creativecommons.org/licenses/by-nc/4.0/ ) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Inadequate glycemic control usually leads to peripheral neuropathy, vasculopathy, and foot deformities that leads to diabetic foot ulcer (DFU), and a 10-years history of diabetes and inadequate self-management increases the risk of reoccurring DFU. A home-based intervention program, which includes Diabetes Self-Management Education (DSME) and wound care is the most likely approach, to engage families and overcoming the barriers in self-care management. The aim of this study is to provide an overview on the effectiveness of home-based nursing intervention in the elderly patients with reoccurring diabetic foot ulcers.
Design and method: In this study, a case study approach was used that presented a case related to self-management and wound care in elderly patients with reoccurring DFU. The intervention was carried out by the community health nurses for eight weeks with home visit.
Results: Significant changes were reported in diabetes selfmanagement practices, blood glucose level, and wound healing. The Diabetes Self-Management Questionnaire (DSMQ) score increased from 5.62 to 8.,54 and the Summary of Diabetes Self- Care Activities (SDSCA) score increased from 3.2 to 6. The Bates Jansen Examination score decreased from 24 and 26 to 17 and 14 in six weeks.
Conclusions: The results confirm that family-based interventions program are effective in improving glycemic control and wound healing. Community nursing is believed to prevent an increase in self-management behavior to prevent recurring DFU and maintain a healthy life-style about diabetes self-management education.
Significance for public health.
Diabetes mellitus (DM) with diabetic foot ulcer significantly contributes to the deterioration in health and financial burden on the patient. The increased risk of diabetic foot ulcers, especially in elderly patients with inadequate glycemic control tends to increase diabetes complications and mortality. Furthermore, the functional impairment, cognitive dysfunction, and poverty caused by the aging process make it difficult for elderly people to access health services. Home-based interventions carried out by community health nurses using the patient-centered care approach have advantages in improving access to services. Focusing on the self-management with Diabetes Self-Management Education (DSME) and wound care management to improve glycemic control, optimize the healing process, and also improve health promotion to prevent recurrent diabetic foot ulcers. This article provides an overview on the effectiveness of home-based nursing intervention in the elderly patients with recurrent diabetic foot ulcers.
Key words: Home-based intervention, self-care management, foot ulcer recurrence, DSME
Introduction
Diabetes Mellitus (DM) is a metabolic disease with a large increase in prevalence, especially in a developing country. 1 In Indonesia, basic health research reported that the number of DM increased from 6.9% in 2013 to 8.5% in 2018. 2 Self-management is an integral part of diabetes management procedures, 98% of which are self-care procedures that include supporting self-care activities, including self-monitoring of blood glucose, low-fat diet, daily exercise, and implementing strategic to prevent foot ulcers. Research has shown that many of these self-care activities are independent of one another. 3 , 4 Diabetes management practice is not only complex but also demanding, therefore majority of the patients find it difficult to modify lifestyle and to achieve important physical and psychological impact. 5 With the highest prevalence in incidence, older patients with diabetes encountered many difficulties in self-care activity due to aging process, such as cognitive dysfunction, functional impairment, polypharmacy, vision, and hearing impairment, and depression. 6 In addition, caregivers or families of older people should be included in the intervention program in order to improve self-management behavior. A home based intervention programs for self-management education with Diabetes Self-Management Education (DSME) showed significant effect in glycemic control, self-efficacy, and psychosocial improvements. 7-9
The rise in blood glucose level in the elderly usually leads to complications of various pathophysiological systems, such as peripheral neuropathy, vasculopathy, and foot deformities that lead to a diabetic foot ulcer (DFU). 9 , 10 DFU are classified as chronic, non-healing wounds that create a disruption or an injury to skin layers, necrosis or gangrene that usually occur on the soles of the feet, as a result of peripheral neuropathy or peripheral arterial disease. Sensory neuropathy is the main and most important causative factor, which is usually deep (>50%) before experiencing a loss of protective sensation resulting in susceptibility to physical and thermal trauma and increase the risk of foot ulcers. 11 DFU risk factors include: male sex, diabetes more than ten years, peripheral neuropathy, abnormal foot structure (bone alterations, calluses, nails thickening), peripheral arterial disease, smoking, history of ulcers or amputation, and inadequate glycemic control. 12 As the incidence of diabetes increases, it also predict an increase in complications in diabetes such as DFU, which affects approximately 15-25% of diabetics during lifetime. 13 , 12 With a global prevalence of 6.3%, DFU is the precursor to approximately 85% of the lower extremity amputation. 14
Diabetic patients with DFU also associated with peripheral arterial disease (PAD), increased mortality, reduced mobility, poor psychosocial adjustment, and reoccurrence of ulcer. 15 , 16 caused by biological, physical or behavioral factors, such as increased plant stress, loss the “gift of pain” which leads to lack of appropriate preventive measures, and no follow-up care to identify warning signs of recurrence. Treatment of reoccurring diabetic foot ulcer required adequate glycemic control, ongoing professional foot care at intervals of 1 to 3 months and properly fitting footwear. 16 The ability to identify patients at high risk of this complication can help healthcare providers focus on preventive interventions. The patient education program in treatment of hyperglycemia and integrated foot care is also an important factor to prevent foot ulcer pain. Treatment of hyperglycemia and appropriate wound care management will decrease the complications of DFU. The aim of this study is to provide an overview on the effectiveness of home-based nursing intervention in the elderly patients with reoccurring diabetic foot ulcers.
Design and Methods
This is a case report, and the participants were selected by purposive sampling and given informed consent to attend this study, which was conducted from November to December 2019. The participant is a 69-year-old male patient diagnosed with diabetes mellitus type 2 in 2005 (15 years). He was on medication, using metformin 500 mg twice daily and the last visit to the physician was 5 months ago, and considering visitation for medical services just in case there is a symptom and buying medicine from a pharmacy (refers to an old recipe). There is no dietary abstinence, but the patient said he avoid sugary drinks and limit the consumption of rice. The daily activities are gardening and teaching Qor’an . For the past three months, the average blood glucose level was 198 mg/dl. At the first meeting in home visit, blood glucose in postprandial level = 315 mg/dl and cholesterol level = 198 mg/dl. This high value of blood glucose is influenced by the patient inappropriate habits in taking medication and eating behavior. He said that he did not usually eat breakfast, only consumed cassava or other traditional snacks, which is generally made from wheat or rice flour. He only eats rice during the day and night, in such a way that the medication is taken during the day and night. And often the drugs that must be taken during the day are not taken because they are forgotten. Improper medication and inadequate eating behavior coupled with a lack of physical activity is the main factor for inadequate glycemic control.
The patient has experienced a diabetic foot ulcer twice in the last three years and suffered amputation in-ring toe two years ago. Due to his present condition, he has experienced a diabetic wound in his left foot since last month. From Figure 1 , it can be concluded that the location of his wound is in his sole and pinkie toe. The wound examinations are grade 2 in his pinkie toe, while the wound in his sole-foot is in grade 1 (Wagner classification). There was callus but the stink is not reported, edema in the left foot, dry skin, and the integument color is dark (not like the other’s skin). Bates Jensen Examination of the wound in sole foot with total score = 24 and wound in pinkie toe with total score = 26. There was edema in the left foot. From observation and interview, it was discovered that the patient has a habit of sitting with one of the legs (especially leg with diabetic foot ulcer) raised in the chair or crossed the legs. The activity in teaching Qor’an was carried out by sitting in a cross-legged position with a duration of 2-3 h daily. This position affects blood circulation, which reduces blood flow to the legs area, especially the area with diabetic foot ulcers, and can hinder the healing process.
Nursing care is provided by scheduling a visit to homes twice a week for 6 weeks. Intervention was carried out by DSME and also wound care. Patient and family member as caregiver consisting of wife and daughter involved in health education. DSME delivered information about self-management, which includes understanding diabetes, healthy eating, physical activities, understanding and monitoring blood glucose, medication adherence, problem-solving, coping, and foot care. The education program used interactive discussions and exchange of experiences related to self-management. Education about medication is delivered by teaching and supporting the patient with pill container and record the activity in the medication logbook, which was evaluated by a nurse on a weekly basis. In terms of diet management, the carbohydrate counting method is used to assess the patient carbohydrate requirement and measure the portion of meals daily. This result is complemented by creating a meal schedule with a menu tailored to patient eating habits and recorded in the logbook. The physical activity recommendation was carried out in the fourth week after reduced edema by doing light physical activity by stretching and brisk walking every morning after praying ( Shubuh ) for 30 min daily. The ability of self-care was measured by the Diabetes Selfmanagement Questionnaire (DSMQ), blood glucose level, and The Summary of Diabetes Self-Care Activities Measure (SDSCA) before and after the intervention.
Wound care management consists of wound care practice with modern dressing. A low adherence dressing helps in distributing the fluid, and for the edema in the left foot, a bandage was used for compression. In the fifth week, alternative wound care materials are used, such as honey as a bandage and baby soap as a wound washer, to reduce costs due to the patient’s economic situation. The patient was also encouraged to perform regular foot care, which includes washing of foot regularly, changing the sitting habit, and wearing fitting footwear during daily activities. The management of DFU was measured by the total score of Bates Jansen Examination before and after the intervention.

First inspection of wound (5 November 2019).
Results and Discussions
Table 1 lists the DSMQ and SDSCA scores, which describe the knowledge, attitudes, and practice of self-management. The DSMQ score in the first assessment describes that the patient ability to carry out self-care activities is quite good. The highest DSMQ score is for diet control and health care on the subscale and the lowest is for physical activity and glucose management on the subscale. The patient’s nearly 15-year history in DM provides an opportunity to understand the disease and experience in terms of autonomous management. The patient is experienced in identifying hyperglycemic conditions by noticing the symptoms, namely frequent urination and drowsiness in such a way that they respond to taking medication. However, this was not followed by other self-maintenance behaviors, such as diet and physical activity because they felt that taking medication alone was enough to overcome the disease. Health education that is delivered with discussion strategies and sharing experiences has a good impact on the implementation of patient-centered care strategies. This strategy provides the opportunity for nurses to provide interventions in accordance with the patient conditions. There was a significant increase in the DSMQ score after training at week 6 with a score of 8.54 and a better score on all four subscales. In terms of practice with SDSCA, the scoring before intervention was low with the lowest indicator as physical activity, foot care, and diet. The results after intervention increased with more regular self-management practices after being controlled by the nurse and caregiver. Better self-management practices include taking medications on a timely basis, maintaining regular foot care, and healthy eating habits. In terms of physical activity, the program is limited to walking due to a diabetic foot ulcer.
DSMQ and SDSCA pre and post DSME.
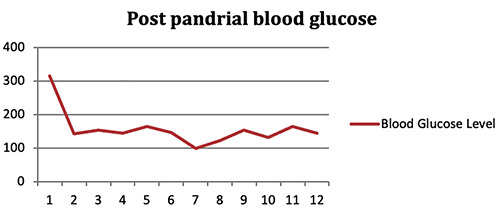
Blood glucose level.

Wound on 16 November 2019.
Figure 2 contains a description of the blood sugar level, which shows the significant decrease in value and stability in 12 measurements (twice a week for 6 weeks). This suggests that blood sugar control has improved along with better self-management practices, especially in regard to taking medication and diet management. The development in 2 weeks of wound care management in Figure 3 showed that compression reduces the edema. The patients were thought how to apply virgin coconut oil (VCO) to optimize moisturizer in dry skin. During 4 weeks of wound care practice in figure 4 , the result showed changes that were consistent with wound examination, that is a total score of Bates Jansen Examination of the wound in sole foot is = 14. And the wound in the pinkie toe has total score = 17. For the following weeks, baby soap was recommended and honey as a substitution for washing and dressing. This product is easy to obtain, cheap, and easy to use. The wound has changed in size, depth, cave size, the decreasing in necrosis tissue, skin color around the wound by decreasing callus. However, there was little development for the blood circulation (edema), and the problem was bad habits in patient behavior, which includes nonmaintenance of the bandage (removed when bathing), that does not change the activity especially in sitting position, or not maintaining the elevation of the foot. It is important to inform the patient on the use bandage, and other bad habits that must be changed by the patient sitting habits and activities that cause blood flow obstruction, for example, posture while sitting, standing, and keeping the legs higher with the pillows while sleeping. The adherence in nursing advice increased in 3 rd week after regular supervision from nurse and caregiver. It was discovered that the compliance of patients and family to keep maintaining bandage is the important factor to reduce edema.
Health education is an effective strategy to improve self-care skills including self-management behavior, HbA1c, and blood sugar control, body weight, improve quality of life, decrease stress and increase adherence to medication behavior. 4 , 5 , 17-19 Therefore, health education with DSME provides an advantage for patients in order to optimize the 3 components of behavior in self-care of chronic illness. According to the research conducted by Abdulrahman et al. 20 provides results that increasing knowledge with health education will increase understanding on the importance of self-care followed by increased behavior. Although health education has a great impact on patient perception, in some condition there is poor understanding in patient especially those with low education and cognitive impairment, such as elderly. When the information is not well communicated by the healthcare professional, patients can have different perceptions and draw their own conclusions. 21 In this case, the patient has a misunderstanding of the correct schedule because, according to the patient, nutrition is only included in rice consumption, although he has a snack in the morning that contain carbohydrate but did not think that he must be taking medication. The health education must consider patient perception in such a way that the nurses can give better strategies to delivered information with proper communication techniques. After an intervention with DSME, changes in self-maintenance behavior can be improved by direct supervision on weekly basis uses a logbook. Home-based intervention program gives an advantage for nurses because they are more informed about habits, direct observation of behavior, more time for education, and involving families in the intervention. 7 , 22 The results support the value of family-based interventions to improve diabetes selfmanagement. 22 The important thing is to integrate DSME in home visit program according to the national program and to adapt the teaching material to the socio-economic context, and to culture and literacy level of the target groups. 23
Wound care is a large part of the growing workload of community nurses, especially with DM-related wounds. There is a need to find a simple and inexpensive product that can be administered to patients for self-care, therefore reducing the workload of the nurse’s and encouraging patients to participate in the wound healing process. For product availability and ease of use, regular salt and soap are safe, simple, and do not cause harm or allergies when compared to povidone iodine and normal saline. 23 This method does not need long-term hospitalization and reduces expenses. Soap is an antiseptic substance and there is no soap-related harm reported till now, and no complications have been reported with water and soap. 23 The other product used for wound care is honey, and Medicinal honey products are an excellent resource for nurses in the community because of the bandages’ multifactorial effects, which often leads to being referred to as all-in-one prep bandages and effective wound bed preparation. These include antimicrobial action, deodorization, pH-modulating agent, debridement, antiinflammatory action, scar reduction, stimulation of new tissue growth (angiogenesis), biofilm control effect, pain management. 24
Early detection and case finding is an important factor in reducing the risk of diabetic foot recurrence. Assessment of knowledge, history of ulcer, and behavior are important factors in determining effective interventions. Patients’ beliefs regarding the symptoms of ulceration and their perceived personal control over ulceration are important determinants of foot care. 25 Increasing knowledge and life-style modification practice include healthy eating, foot care, and properly fitting footwear are predicted to prevent foot ulcer recurrence. 16 Adequate glycemic control, regular foot care and early detection of the symptom recurrence such as a new lesion, callus, and foot deformities are key component included in DSME.
Conclusions
Home-based interventions play an important role in improving patient and family self-care management with mobility impairment due to DFU and the elderly. Strengthening families through involvement in each intervention can help assist patient with monitoring. Understanding the reasons for the recurrence of diabetic ulcers by early assessment of biological and behavioral factors is important to prevent the remission. Increasing foot care practices and behavior changes are the key component to reduce the risk of ulcer recurrence and reduce the burden on patient and families.

Wound on 30 November 2019.
Acknowledgement
The authors express profound gratitude to all those that contributed to the completion of the study. Many thanks to the patient for the willingness to participate. Thanks to Sukmajaya Primary Health Care, Faculty of Nursing Universitas Indonesia and School of Nursing, Faculty of Medicine, Universitas Brawijaya for the support during this study.
Funding Statement
Funding: This study was financially supported by Faculty of Medicine Brawijaya University Malang.
- 1. Wu Y, Ding Y, Tanaka Y, et al. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci 2014;11:1185–200. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Ministry of Health Republic of Indonesia. Basic Health Research 2018. Jakarta: Ministry of Health Republic of Indonesia; 2018. [ Google Scholar ]
- 3. Jannoo Z, Mamode Khan N. Medication adherence and diabetes self-care activities among patients with type 2 diabetes mellitus. Value Heal Reg Issues 2019;18:30–5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Yuan C, Lai CW, Chan LW, et al. The effect of diabetes selfmanagement education on body weight, glycemic control, and other metabolic markers in patients with type 2 diabetes mellitus. J Diabetes Res 2014;2014:789761. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Trevisan DD, São-João T, Cornélio M, et al. Effect of an 'implementation intention' intervention on adherence to oral anti-diabetic medication in Brazilians with type 2 diabetes. Patient Educ Couns 2020;103:582-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care 2012;35:2650-64. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. García AA, Brown SA, Horner SD, et al. Home-based diabetes symptom self-management education for Mexican Americans with type 2 diabetes. Health Educ Res 2014;30:484–96. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Davis WA, Lewin G, Davis TME, et al. Determinants and costs of community nursing in patients with type 2 diabetes from a community-based observational study: The Fremantle Diabetes Study. Int J Nurs Stud 2013;50:1166–71. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Felix HC, Narcisse MR, Long CR, et al. The effect of family diabetes self-management education on self-care behaviors of Marshallese adults with type 2 diabetes. Am J Health Behav 2019;43:490–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Handayani E. Modern wound care application in diabetic wound management. Int J Res Med Sci 2017;5:702–6. [ Google Scholar ]
- 11. Gnanasundaram S, Ramalingam P, Nath B. Gait changes in persons with diabetes: early risk marker for diabetic foot ulcer. Foot Ankle Surg 2020;26:163-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Rosyid FN. Etiology, pathophysiology, diagnosis and management of diabetics’ foot ulcer. Int J Res Med Sci 2017;5:4206–13. [ Google Scholar ]
- 13. Tresierra-Ayala MÁ, García Rojas A. Association between peripheral arterial disease and diabetic foot ulcers in patients with diabetes mellitus type 2. Medicina Universitaria 2017;19:123–6. [ Google Scholar ]
- 14. Yazdanpanah L, Shahbazian H, Nazari I, et al. Diabetes & metabolic syndrome: Clinical research & reviews risk factors associated with diabetic foot ulcer-free survival in patients with diabetes. Diabetes Metab Syndr Clin Res Rev 2018;12:1039–43. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Gianino E, Miller C, Gilmore J. Smart wound dressings for diabetic chronic wounds. Bioengineering (Basel) 2018;5:51. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med 2017;376:2367–75. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Yu CH, Parsons JA, Mamdani M, et al. A web-based intervention to support self-management of patients with type 2 diabetes mellitus: Effect on self-efficacy, self-care and diabetes distress. BMC Med Inform Decis Mak 2014;14:117. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Nwankwo CU, Ezenwaka CE, Onuoha PC, et al. Implementing diabetes self-management education (DSME) in a Nigerian population: Perceptions of practice nurses and dieticians. Arch Physiol Biochem 2015;121:123–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Lavelle D, Zeitoun J, Stern M, et al. Diabetes self management education in the home. Atl Heal Syst 2016;8:1–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Abdulrahman M, Husain ZSM, Abdouli KA, et al. Association between knowledge, awareness, and practice of patients with type 2 diabetes with socio-economic status, adherence to medication and disease complications. Diabetes Res Clin Pract 2020;163:108124. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Lukman NA, Leibing A, Merry L. Self-care experiences of adults with chronic disease in Indonesia: An integrative review. Int J Chronic Dis 2020;2020:1–17. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Dube L, Van den Broucke S, Dhoore W, et al. An audit of diabetes self-management education programs in South Africa. J Public Health Res 2015;4:581. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Najafian A, Fallahi S, Khorgoei T, et al. Role of soap and water in the treatment of wound dehiscence compared to normal saline plus povidone-iodine: A randomized clinical trial. J Educ Health Promot 2015;4:86. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Evans J. A solution to cost-effective wound management in the community. J Comm Nurs 2014;28:46-51. [ Google Scholar ]
- 25. Vedhara K, Dawe K, Wetherell MA, et al. Illness beliefs predict self-care behaviours in patients with diabetic foot ulcers: a prospective study. Diabetes Res Clin Pract 2014;106:67-72. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (232.8 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

A 57-Year-Old Man with Type 1 Diabetes Mellitus and a Chronic Foot Ulcer Successfully Managed with a Remote Patient-Facing Wound Care Smartphone Application
Ling yuan kong, jose luis ramirez-garcialuna, robert d j fraser, sheila c wang.
- Author information
- Article notes
- Copyright and License information
Corresponding Author: Sheila C. Wang, e-mail: [email protected]
Authors’ Contribution:
Study Design
Data Collection
Statistical Analysis
Data Interpretation
Manuscript Preparation
Literature Search
Funds Collection
Ling Yuan Kong and Jose Luis Ramirez-GarciaLuna contributed equally to this work
Financial support: None declared
Conflict of interest: LYK has no conflicts of interest to declare. JRG holds a Mitacs Elevate Postdoctoral Fellowship in conjunction with McGill University as Academic Partner and Swift Medical as Industrial Partner. RF is an employee at Swift Medical. SCW is a co-founder, shareholder, and Chief Medical Officer of Swift Medical, Inc; she currently receives no compensation from the company. All author’s roles in the project were not on behalf of any of the mentioned company or entities but rather in the context of their academic appointments/affiliations
Received 2021 Jul 5; Accepted 2021 Oct 27; Revised 2021 Nov 8; Collection date 2021.
This work is licensed under Creative Common Attribution-NonCommercial-NoDerivatives 4.0 International ( CC BY-NC-ND 4.0 )
Patient: Male, 57-year-old
Final Diagnosis: Diabetic foot
Symptoms: Chronic ulcer • osteomyelitis • polymicrobial infection
Medication: —
Clinical Procedure: Bone scan • intravenous antibiotic • oral antibiotic • PET-CT • telemedicine
Specialty: Dermatology • Infectious Diseases • Podiatry
Unusual setting of medical care
Background:
Wounds affect millions of people world-wide, with care being costly and difficult to deliver remotely. The ongoing COVID-19 pandemic highlights the urgent need for telehealth solutions to play a larger role as part of remote care strategies for patient monitoring and care. We describe our findings on the use of a patient-facing wound care app (Swift Patient Connect App, Swift Medical, Canada) as an innovative solution in remote wound assessment and management of a diabetic patient’s wound.
Case Report:
In February 2020, a 57-year-old man with type I diabetes and peripheral arterial disease presented with osteomyelitis in the left foot at the fifth metatarsal, arising from a chronic ulcer. The wound was deep, with purulent discharge and polymicrobial growth. A 6-week course of intravenous antibiotics was administered, with slow improvement of the wound. At a follow-up appointment in June 2020, The Patient Connect app was recommended to the patient to securely share calibrated images of his wound as well to communicate with his doctor. Between June 2020 and January 2021, wound closure was accurately monitored as part of the management of this diabetic foot infection. The app was also used in the management of 2 subsequent wounds and infection episodes.
Conclusions:
Use of the Swift Patient Connect App designed to monitor and manage wounds by a patient with diabetes and foot ulcer as part of a remote care strategy resulted in numerous benefits expressed by the patient. After initial adoption, 3 successive wounds were managed with a combination of in-person and telehealth visits complemented by the app. Incorporation of this technology as part of a novel telemedicine strategy promises to have an extensive impact on remote care delivery during the current COVID-19 pandemic and beyond.
Keywords: Artificial Intelligence, Diabetic Foot, Telemedicine, Wounds and Injuries
Wounds affect millions of people world-wide, with care being costly and difficult to deliver remotely [ 1 ]. A major limitation in the delivery of telemedicine remains the difficulty that many doctors and care providers experience with being able to conduct adequate visual assessments of patient wounds remotely [ 2 ]. Currently, standard telehealth practice involves patients using their smartphones to transmit photographs of their wounds through direct messaging services to their care provider; such images are often poorly calibrated for size, color, and lighting, not to mention the lack of security using such an approach. Wound-related information is either communicated over telephone or through text messages, which suffers from a lack of standardization of descriptors for issues such as pain and presence of exudate. Therefore, for remote care delivery to match the level received through in-person appointments, there is an urgent need for patients to be able to easily capture high-quality images of their wounds, that also contains high-quality information content which can be securely shared.
Healthcare apps are specially designed applications for smart-phones with health-oriented functionality [ 2 ]. By one estimate, over 318 000 health-related apps are available for download [ 3 ]. The US Food and Drug Administration (FDA) defines software functions such as those found in mobile medical apps as “device software functions” ( https://www.fda.gov/media/80958/download ). In addition, to assist with adhering to relevant design, best practices, and usage considerations, the World Health Organization (WHO) has published guidelines on digital health interventions ( https://www.ncbi.nlm.nih.gov/books/NBK541905/ ). Evidence from 2020 during the COVID-19 pandemic suggests it played a pivotal role in the widespread implementation of digital technologies in healthcare [ 4 ]. We previously developed a mobile app and dashboard (Swift™ Skin and Wound) specifically designed to accurately and reliably measure and document many aspects of wounds [ 5 ] ( Figure 1A–1D ). The system, which is registered as a clinical device with Health Canada ( https://health-products.canada . ca/mdall-limh/dispatch-repartition.do?type=active) and the US FDA ( https://fda.report/Company/Swift-Medical-Inc ), uses machine-vision technology to automatically focus and calculate wound dimensions from images acquired by a smartphone’s camera, allowing users to obtain precise and consistent measurements. These capabilities have been demonstrated to reduce the time needed for and increase accuracy of patient wound assessments compared with the traditional paper-and-ruler method [ 6 ].
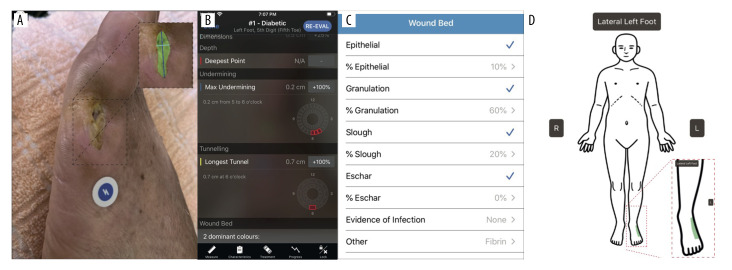
Patient wound imaging, measurements, and progression tracking using the Swift Medical™ Skin and Wound App and Dashboard. ( A ) Example image of patient wound, taken using the Skin and Wound app. The app uses an adhesive fiducial marker (HealX™ calibrant), a Health Insurance Portability and Accountability Act, 1996 (HIPAA)-compliant, FDA and Health Canada certified Class I medical device placed next to the wound to automatically focus and acquire high-quality images, calibrate for color, lighting, and distancing when imaging. Note the image’s color calibration and focus. AI is used to automatically define the wound’s surface area (expanded box with wound area artificially shaded in green). All images are encrypted and stored in secure, cloud-based servers. ( B ) Screen shot showing wound-related metrics calculated by Skin and Wound app’s AI. ( C ) Image of wound-bed-related information taken from the dashboard. The app enables remote monitoring of high-risk individuals, offering insights into the healing process, including the tissue type present and its area. Patient identifiers (eg, name and unit number) are also accessible through the app’s dashboard, and treatment advice and care-related communications can be provided directly to the patient. ( D ) Human silhouette accessible through the HIPAA-compliant Skin and Wound healthcare provider dashboard showing the anatomical location of the wound, imaged by the patient.
In response to the increased reliance on remote appointments brought about by the COVID-19 pandemic [ 7 ], we have recently developed a stream-lined, patient-facing version of the app (Patient Connect, Figure 2A, 2B ), designed for use by patients and/or their care providers using their own personal smartphones. In addition to being able to view a wound’s image series over time, additional information such as healing-associated metrics, wound-bed information, anatomical location, and patient identifiers can be viewed. We report the case of a patient with diabetes and multiple episodes of foot infections who was successfully managed using this app during the COVID-19 pandemic in 2020-2021. As well as reporting on their experiences, we present evidence demonstrating the app’s effectiveness in both remote care management and delivery.
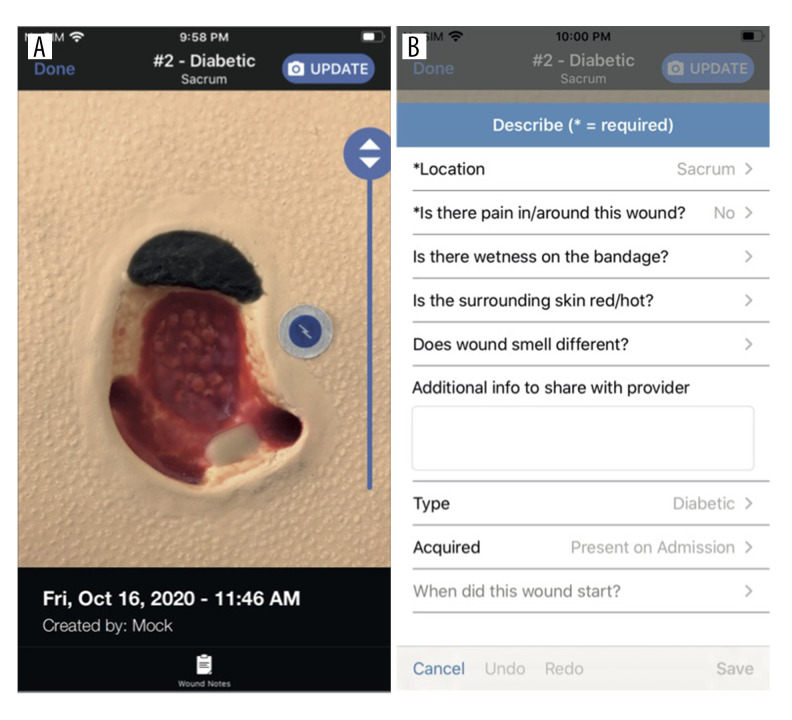
Swift Medical Patient Connect App Interface . ( A ) Screen shot of an artificial wound captured using the Patient Connect App, which has more limited functionality compared to the Skin and Wound app: for example, wound measurements cannot be accessed by the patient/user of the Patient Connect app. ( B ) Screen shot of the Patient Connect app dashboard, indicating qualitative information fields that can be populated by the patient/user.
Case Report
In February 2020, a 57-year-old man with type I diabetes, coronary artery disease, chronic kidney disease, peripheral arterial disease, and prior toe amputation for infection presented with osteomyelitis in the left foot at the fifth metatarsal, arising from a chronic ulcer. The patient did not smoke, drink alcohol, or use recreational drugs. The wound was deep, with purulent discharge and polymicrobial growth, which included Pseudomonas aeruginosa . A 6-week course of intravenous ertapenem 500 mg (once daily) and oral ciprofloxacin 250 mg (twice daily) was administered, with slow improvement in the wound.
Between the patient’s first visit in February 2020 and early June 2020, he was followed via telephone at regular intervals.
The attending physician and patient mutually agreed that the patient would provide photos via direct communication (text message or email) to allow wound assessment: despite ethical concerns regarding the sharing of the physician’s personal contact information, this was deemed crucial given the patient’s need for close follow-up and their reluctance to present for in-person follow-up in the pandemic context. During this 3-month period of remote follow-up, the patient shared 2 photographs of the wound: an example is shown in Figure 3A .
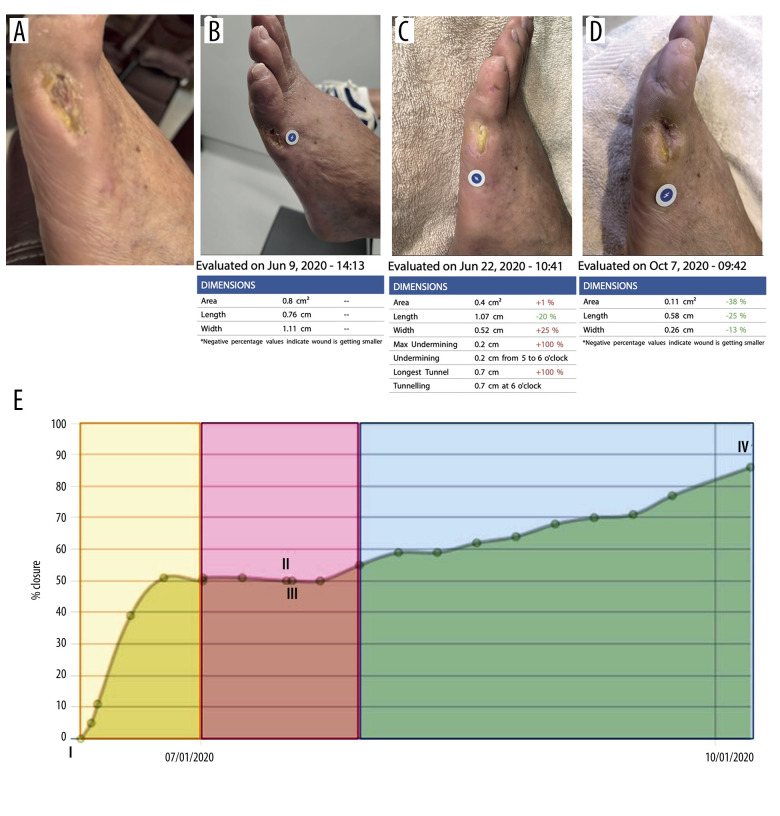
Patient wound monitoring using the Skin and Wound platform. ( A ) Baseline photograph of patient’s wound associated with underlying osteomyelitis. Image was taken using the standard iPhone Camera App on an iPhone11 running iOS 14.0.1 and is representative of the 2 photographs shared by the patient between February and June 2020. Note the image’s lack of focus. The patient shared 2 images using the Camera App. ( B ) Image of the dashboard showing wound image and healing process-associated metrics, acquired on the date and at the time indicated. ( C ) Same as B except at the later date indicated. ( D ) Same as C , except at the later date indicated. ( E ) Closure graph viewed through the dashboard, automatically calculated from aggregated images of the wound over time. I, II, and IV indicate the dates when the images shown in B–D were captured. The timeframe highlighted in yellow indicates when the patient received antibiotics, which corresponded to enhanced healing of the wound. After the healing stalled (highlighted in pink), a tunnel wound was detected (III), resulting in wound debridement and the insertion of a mesh. This was followed by further closure of the wound (highlighted in blue). At IV, wound closure was calculated at 86%.
In June 2020, the patient reported pain and new discharge from the wound, which prompted an in-person visit on June 9, 2020. A bone and PET scan showed resolution of osteomyelitis, with soft-tissue inflammation. He was treated with another course of oral antibiotics (amoxicillin-clavulanate and ciprofloxacin). At this point, the patient agreed to download and use the Swift Medical Patient Connect App to capture and share images of the wound ( Figure 3B–3D ). As of January 2021, the patient had 7 additional telemedicine appointments and submitted a total of 39 images through the app, an almost 20-fold increase in sharing wound-related data compared to the situation before using the app. The wound gradually improved over this time, with objective decrease in size as measured by the app ( Figure 3E ). The patient subsequently developed 2 additional wounds in different locations and was followed again via the app, with ongoing use as of September 2021. Throughout a 1-year period as part of telehealth care, the app permitted the longitudinal monitoring and successful management of 3 infection episodes in a high-risk patient.
As wound assessment via the app occurred weekly, formal monitoring increased self-examination and engagement in preventive behavior such as monitoring for trauma and early signs of infection and off-loading wound pressure using orthotics. Owing to the patient’s comorbidities and the pandemic, he was reluctant to attend in-person appointments. Use of the app therefore reduced anxiety through reduced healthcare contact and surrounding risk of hospital-associated COVID-19 exposure. From the physician’s perspective, the increased frequency of images provided by the patient for review allowed real-time assessment of the wound, increasing physician confidence in remote wound monitoring.
Use of the Patient Connect App also helped realize time and cost savings. Total time and financial commitment from the patient per appointment averaged 3 hours and approximately $50 CAD, respectively: remote appointments eliminated both of these costs. For the physician, use of the Patient Connect App as part of the remote care strategy deployed resulted in a substantial time saving: the standard workflow ordinarily required to visually assess the wound, including positioning, dressing removal, and cleansing, was eliminated. The physician estimated that this reduced the time required from 30 to 15 minutes: if this modality were widely adopted, this would potentially allow twice the number of patients to be seen. In addition, the patient captured photos during visits by a local community service centre nurse who performed his routine dressing changes. As regular dressing changes remain an essential part of wound care, whether delivered in-person or remotely, the ease of imaging the wound as part of routine wound care in a standardized manner represented another time-saving factor.
The COVID-19 pandemic has placed great importance on the use of novel strategies for remote care of patients [ 4 ]. Regular use of the Patient Connect App by the patient in this case report allowed remote monitoring of the wound and could potentially promote higher rates of adherence to treatment through engagement in preventive care and early wound detection. Access to the Patient Connect App is provided through a health care provider that has access to the Swift Medical solution through a licensing agreement; the Patient Connect App itself is free and there is no charge to the patient or caregiver using the app. The virtual appointments had no upfront cost for the patient, and the physician was remunerated for virtual visits via the healthcare system, similar to in-person visits, through a separate billing code.
Factors that would help the widespread adoption of this innovation include more evidence-based research from larger patient populations to demonstrate the app’s effectiveness and benefits in helping deliver remote care; patient education on the use of apps and general improvements in the familiarity of certain population groups (eg, the elderly) with technology; and access to high-speed internet, especially for rural/indigenous populations.
In the case reported, the patient explained that he shared an increased number of images because he felt comfortable using a formal, specially designed portal through which the physician was able to access images at their convenience. The patient found the app “educational and empowering”, consistent with an earlier study on patient wound-perception [ 8 ]. This observation is also consistent with a recent study describing the use of an mHealth tool facilitating remote assessment of digital ulcers, resulting in high levels of patient satisfaction [ 9 ]. Possession of and familiarity with a smartphone is an obvious pre-requisite for using this technology, but given their ubiquity, we do not envision this being a significant limitation. Presently, the Patient Connect App is being used in addition to other care practices, including telephone calls and in-person visits, which remain essential in the care of patients with wounds. If the app were to completely substitute for in-person visits, a major concern remains whether complications might be missed or wounds mis-diagnosed, resulting in administration of inappropriate treatments. Therefore, more research is required to determine if this innovation can provide a level of patient care comparable to standard care/ in-person appointments.
Telemedicine strategies have increasingly been used to monitor and treat diabetic foot ulcers (DFUs) [ 10 ]. A recent systematic review showed that photographic imaging of wounds is a valid, reliable, and feasible method for telehealth purposes [ 11 ]. At-distance photographic imaging of wounds is associated with good levels of patient adherence and timely referrals based on photographic assessments, thus leading to a favorable perception of usability [ 12 ]. However, the lack of consistent imaging regarding scale, focus, and lightning conditions has been tied to relatively low inter- and intra-observer reliability in the diagnosis of DFU complications based on mobile phone imaging [ 13 ]. Another systematic review [ 14 ] found that the use of mobile applications for monitoring DFUs led to increased community support and wound care knowledge, and helped empower patients. The study also concluded that a lack of technological savviness, non-user-friendly or non-intuitive apps, and lack of patient dexterity were significant hurdles to the widespread adoption of wound-care mobile applications.
A common concern over the use of smartphones as part of remote care strategies remains the security of patient data [ 15 ]. Prior to using the app, despite being able to directly contact the physician, the present patient considered sending images a potential imposition on the physician. The patient also felt uncomfortable that images would be sent via standard messaging and stored on the physician’s smartphone. In contrast, by storing images captured using the app on secure cloud-based servers, this reduced the patient’s anxiety about sharing images and facilitated the physician’s ability to rapidly and securely receive images. In addition, patient identifiers (eg, name and unit number) are accessible through the secure dashboard, and treatment advice and care-related communications can be provided directly to the patient using the app.
The Patient Connect App can be used by any patient treated for any condition involving a wound or skin condition that requires monitoring. Underscoring this point, the app is being used not only where we are based at McGill University Health Centre by colleagues and collaborators in the Division of Orthopedic Surgery and Diabetic Clinic, but has also been implemented at other hospitals such as the Jewish General Hospital, where this patient was treated, and in ambulatory settings (Ostomy care and pressure ulcer prevention, Centenary Hospital; Scarborough Health Network; Saint Elizabeth Health, Home and Community Care Support Services Central East; The Michener Institute; University Health Network) throughout Quebec and Ontario. In addition, the Patient Connect App has recently been licensed to a national health care system in the US, with the contract able to support up to 10 000 patients, which will ensure its impact in the short-to-medium term. Studies are underway to more rigorously determine the extent of time savings made through use of the app (eg, average number of days lost due to unplanned hospital admissions) and to investigate whether use of the app as part of a remote wound care strategy can deliver care comparable to or better than standard care/in-person appointments.
Conclusions
Here, we present the case of a 57-year-old man with type 1 diabetes mellitus and a chronic foot ulcer who was successfully managed with a remote patient-facing wound care smart-phone application. The use of an innovative patient-facing smart phone app designed to monitor and manage wounds by a patient with diabetes and foot ulcer resulted in numerous benefits. After initial adoption, 3 successive wounds were managed with a combination of in-person and telehealth visits complemented by the app. Incorporation of this technology as part of a novel telemedicine strategy promises to have an extensive impact on remote care delivery, during the current COVID-19 pandemic and beyond.
Department and Institution Where Work Was Done
Division of Infectious Diseases, Jewish General Hospital, Montreal, QC, Canada.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1. Guest J, Fuller GW, Vowden P, et al. Cohort study evaluating pressure ulcer management in clinical practice in the UK following initial presentation in the community: costs and outcomes. BMJ Open. 2018;8(7):e021769. doi: 10.1136/bmjopen-2018-021769. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Wang SC, Au Y, Ramirez-GarciaLuna JL, et al. The promise of smartphone applications in the remote monitoring of postsurgical wounds: A literature review. Adv Skin Wound Care. 2020;33(9):489–96. doi: 10.1097/01.ASW.0000694136.29135.02. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. IQVIA The Growing Value of Digit al Health: Evidence Impact on Human Health the Healthcare System Institute Report. IQVIA; 2017. Available at: https://www.iqvia.com/insights/the-iqvia-institute/reports/the-growing-value-of-digital-health .
- 4. Golinelli D, Boetto E, Carullo G, et al. Adoption of digital technologies in health care during the COVID-19 pandemic: Systematic review of early scientific literature. J Med Internet Res. 2020;22(11):e22280. doi: 10.2196/22280. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Wang SC, Anderson JAE, Evans R, et al. Point-of-care wound visioning technology: Reproducibility and accuracy of a wound measurement app. PLoS One. 2017;12(8):e0183139. doi: 10.1371/journal.pone.0183139. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Au Y, Beland B, Anderson JAE, et al. Time-saving comparison of wound measurement between the ruler method and the swift skin and wound app. J Cutan Med Surg. 2019;23(2):226–28. doi: 10.1177/1203475418800942. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Webster P. Virtual health care in the era of COVID-19. Lancet. 2020;395(10231):1180–81. doi: 10.1016/S0140-6736(20)30818-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Wang SC, Anderson JA, Jones DV, et al. Patient perception of wound photography. Int Wound J. 2016;13(3):326–30. doi: 10.1111/iwj.12293. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Zhang J, Mihai C, Tüshaus L, et al. Wound image quality from a mobile health tool for home-based chronic wound management with real-time quality feedback: Randomized feasibility study. JMIR Mhealth Uhealth. 2021;9(7):e26149. doi: 10.2196/26149. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Najafi B, Reeves ND, Armstrong DG. Leveraging smart technologies to improve the management of diabetic foot ulcers and extend ulcer-free days in remission. Diabetes Metab Res Rev. 2020;36(Suppl. 1):e3239. doi: 10.1002/dmrr.3239. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Hazenberg CEVB, Aan de Stegge WB, Van Baal SG, et al. Telehealth and tele-medicine applications for the diabetic foot: A systematic review. Diabetes Metab Res Rev. 2020;36(3):e3247. doi: 10.1002/dmrr.3247. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Hazenberg CE, Bus SA, Kottink AI, et al. Telemedical home-monitoring of diabetic foot disease using photographic foot imaging – a feasibility study. J Telemed Telecare. 2012;18(1):32–36. doi: 10.1258/jtt.2011.110504. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. van Netten JJ, Clark D, Lazzarini PA, et al. The validity and reliability of remote diabetic foot ulcer assessment using mobile phone images. Sci Rep. 2017;7(1):9480. doi: 10.1038/s41598-017-09828-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Foong HF, Kyaw BM, Upton Z, et al. Facilitators and barriers of using digital technology for the management of diabetic foot ulcers: A qualitative systematic review. Int Wound J. 2020;17(5):1266–81. doi: 10.1111/iwj.13396. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Gunter RL, Chouinard S, Fernandes-Taylor S, et al. Current use of telemedicine for post-discharge surgical care: A systematic review. J Am Coll Surg. 2016;222:915–27. doi: 10.1016/j.jamcollsurg.2016.01.062. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (1.2 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Probing community nurses' professional basis: a situational case study in diabetic foot ulcer treatment
Affiliations.
- 1 PhD Fellow, Department of Health Science and Technology, Aalborg University, Denmark.
- 2 Associate Professor, Department of Health Science and Technology, Aalborg University, Denmark.
- 3 Charge Nurse, The Wound Healing Knowledge Centre, Bispebjerg Hospital.
- 4 Chief Surgeon, The Wound Healing Knowledge Centre, Bispebjerg Hospital.
- 5 Clinical Head Nurse, The Wound Healing Knowledge Centre, Bispebjerg Hospital.
- 6 Professor, Department of Health Science and Technology, Aalborg University, Denmark.
- PMID: 28252333
- DOI: 10.12968/bjcn.2017.22.Sup3.S46
Complicated and long-lasting wound care of diabetic foot ulcers are moving from specialists in wound care at hospitals towards community nurses without specialist diabetic foot ulcer wound care knowledge. The aim of the study is to elucidate community nurses' professional basis for treating diabetic foot ulcers. A situational case study design was adopted in an archetypical Danish community nursing setting. Experience is a crucial component in the community nurses' professional basis for treating diabetic foot ulcers. Peer-to-peer training is the prevailing way to learn about diabetic foot ulcer, however, this contributes to the risk of low evidence-based practice. Finally, a frequent behaviour among the community nurses is to consult colleagues before treating the diabetic foot ulcers.
Keywords: community nursing; diabetic foot ulcers; knowledge level; professional basis; treatments.
- Clinical Competence*
- Community Health Nursing / education
- Community Health Nursing / standards*
- Diabetic Foot / nursing*
- Education, Nursing*
- Nurses, Community Health*
- Referral and Consultation

IMAGES
VIDEO
COMMENTS
We're going to go through a case study for a diabetic foot ulcer together. Let's get started. In this scenario, Michael is a 15-year-old male diagnosed last year with diabetes type one. He presents to the acute care unit with a sore that will not heal on the bottom of his right foot. ... This nursing case study course is designed to help ...
Approximately between 15 and 25% of diabetic patients will present with foot ulcers throughout their life, this being the main cause of non-traumatic amputation worldwide. The overall prevalence rate of this complication is between 1.3 and 4.8%. These are developed by the convergence of several predisposing, triggering and aggravating factors.
The current study is a case study analysis aimed at evaluating a patient with a diabetic foot ulcer by providing a discussion on effective care management through the use of systematic care planning. This analysis is essential in the identification of crucial care plans that must be provided systematically to improve the quality of life of the ...
Imaging diagnosis of diabetic lower extremity ulcers before treatment for case 1 (A-C) and case 2 (D-F).(A) Picture showed an ulcerated surface on the inner skin of the right calf, about 3.0×2.0 cm in size and 6 mm in depth; (B) MRI showed a local subcutaneous soft tissue defect at the medial margin of the right calf, with swelling in the margin and adjacent soft tissue space; (C) Gray-scale ...
In this case report, providers sought to implement an MDT approach to treat a patient with diabetes and foot ulcers, actively involving the patient's caregiving family members. ... A Multidisciplinary Team Approach for Diabetic Foot Ulcer: A Case Study Adv Skin Wound Care. 2023 Apr 1;36(4):1-4. doi: 10.1097/01.ASW.0000920512.88426.90.
Case Study from Podiatry Today. This author navigates the complex issues in treating an elderly patient with a heavily exudative diabetic foot ulcer, which has recurred over an 11-year period. ... His past history included heavy tobacco use of greater than 60 years and a recently diagnosed onset of type 2 diabetes. The Director of Nursing (DON ...
The aim of this study is to provide an overview on the effectiveness of home-based nursing intervention in the elderly patients with reoccurring diabetic foot ulcers. Design and method: In this study, a case study approach was used that presented a case related to self-management and wound care in elderly patients with reoccurring DFU. The ...
Here, we present the case of a 57-year-old man with type 1 diabetes mellitus and a chronic foot ulcer who was successfully managed with a remote patient-facing wound care smart-phone application. The use of an innovative patient-facing smart phone app designed to monitor and manage wounds by a patient with diabetes and foot ulcer resulted in ...
Diabetes & Primary Care's series of interactive case studies is aimed at all healthcare professionals in primary and community care who would like to broaden their understanding of diabetes.. Around one in three people with diabetes will develop a foot ulcer within their lifetime. Primary care plays a critical role in identifying problems with the diabetic foot, and in responding rapidly and ...
The aim of the study is to elucidate community nurses' professional basis for treating diabetic foot ulcers. A situational case study design was adopted in an archetypical Danish community nursing setting. Experience is a crucial component in the community nurses' professional basis for treating diabetic foot ulcers.