

Proper documentation protects patients and your license
Understand the risks of erroneous and incomplete documentation..
- Nursing documentation with incorrect patient information is responsible for up to 72% of all electronic health record-related risk issues.
- Disciplinary actions from state boards of nursing may be imposed on a nurse in the event of negative patient outcomes resulting from erroneous or missing documentation.
- Nurses can protect their licensure by ensuring their documentation is as complete and accurate information.
Nursing documentation plays a critical role in healthcare. Errors or incomplete information can affect data accuracy and ultimately best practices. Improper documentation also can contribute to adverse, sometimes fatal, patient outcomes. When you document completely and accurately, you reduce your liability risk and have the strongest legal defense in the event of a malpractice lawsuit or licensing board disciplinary action. You face many urgent demands during your shift and charting may seem like a distraction from the work of patient care, but nursing documentation provides essential information to other healthcare colleagues on the patient’s care team and fulfills the nursing professional requirement to maintain a complete care record.
Remembering everything that’s occurred during a shift and every element of care you’ve provided to patients is almost impossible, so your documentation serves as the only record detailing patients’ clinical status and their response to treatments and interventions. One of the most common mistakes made by novice nurses is documentation errors, which most likely result from their intense focus on perfecting clinical skills. Seasoned nurses, on the other hand, face heavy patient workloads and concentrate on completing care tasks during their shift, which may lead them to put this critical aspect of their professional role on the backburner and result in rushed, incomplete, or missing documentation.
Nurse documentation and the electronic health record
Protecting yourself from malpractice claims
Evolution of nursing documentation
When I began my nursing career in 1990, all nurses wrote shift assessments and nursing care tasks in a narrative note, which could take 45 to 60 minutes to complete at the end of my rounds. It was customary to write with black ink on day shifts, green on evenings, and red on nights. To ensure I had all three colors easily available depending on which shift I worked, I taped the pens together. We began using templates a few years later, which saved time by allowing nurses to simply check off assessment findings rather than writing a narrative note.
The adoption of the electronic health record (EHR) now allows nurses to document by clicking checklists on the computer screen with less narrative documentation required. However, although EHR’s provide clinical data for organizations to improve patient safety and evaluate the quality of care, nurses still carry the burden of completing documentation for a large assignment of patients. In 2022, according to Iuppa, inpatient nurses at the Cleveland Clinic spent approximately 123 minutes per shift navigating the EHR.
Document completely and accurately
For over 20 years, my job in quality improvement has involved reviewing patient charts in response to patient complaints or adverse events. Most of these records either lacked pertinent clinical data or vital information about the patient, which didn’t support that the nurse had provided appropriate care. For example, to highlight 10- to 15-minute monitoring of the patient during a shift, a nurse might document the following: “patient on the phone,” “patient off the phone,” and “patient eating dinner.” The nurse may have good intentions, but this doesn’t provide any information on the patient’s clinical status. (See Document clinically, objectively, thoroughly .)
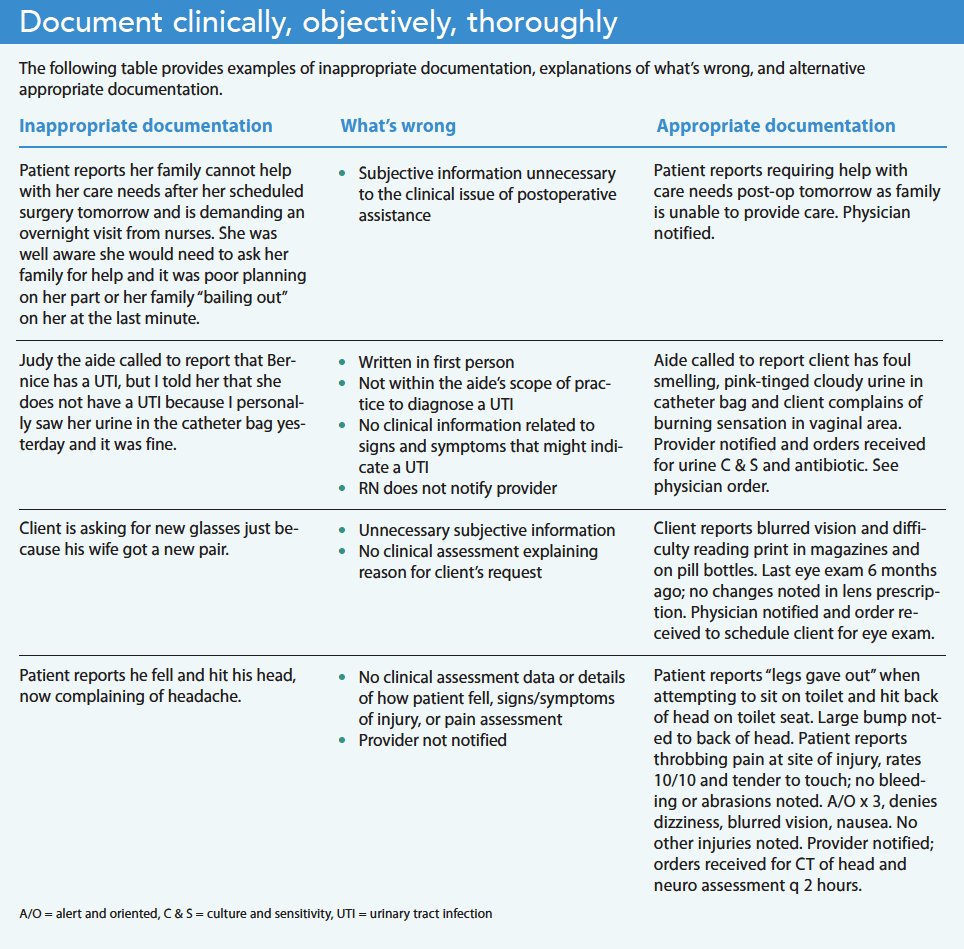
Incomplete documentation also presents a liability risk because it doesn’t provide an accurate description of the patient and may result in serious medical error. Consider this documentation: “Patient sitting on edge of the bed, nose bleeding and urinating on the floor.” Your first thought might be that the patient is experiencing some form of cognitive decline that jeopardizes their safety. This account doesn’t provide any relevant clinical details to explain the cause of the bleeding and urinating. A more informative and accurate documentation of the patient’s status might read as follows: “Patient is alert and oriented with a small amount of bloody drainage noted to the right side of the nose where the patient picked at an old scab. The patient is having difficulty using the urinal at the bedside with urine spilling onto the floor. A bedside commode was placed next to the bed and the patient was instructed to use it when urinating or to call the nurse for assistance. Patient verbalized understanding.” The revised documentation provides not only a precise description of the patient but also important clinical information about the nursing care provided. NurseJournal advises nurses to include the following information when documenting in the EHR:
- Patient health status and drug information
- Medications that have been given and discontinued
- Nursing actions
- Changes in the patient’s condition
- Any orders given regarding the patient’s care
Poor documentation and career consequences
Failure to provide accurate and complete documentation puts you at risk of being named in a malpractice lawsuit, which might take years to resolve and may cause fear and a loss of confidence in your ability to practice as a nurse. I’ve been asked to provide a deposition for a lawsuit only once in my career. I wasn’t named as a defendant, but it was still a nerve-wracking experience. Being quizzed vigorously by the prosecuting attorney about a patient I took care of 5 years earlier isn’t something I want to go through again. If my documentation hadn’t supported the care I provided, the ordeal might have been much worse.
According to liability claim reports published by the insurance provider Coverys in 2021 and the Nurses Service Organization (NSO) in 2020, omissions or errors in nursing documentation were responsible for 72% of all EHR-related risk issues, and the second highest reason for liability claims against nurses. NSO’s analysis of the specific types of allegations related to nursing documentation revealed the following:
- 50% are due to fraudulent or falsified patient records
- 29% are due to failure to document treatment/care required by regulatory agencies
- 13% are due to documentation not accurately reflecting patient care
- 4% are due to inadequate or untimely documentation
Results from a Medscape survey of malpractice respondents found that 14% recognized that better documentation would have helped them avoid a malpractice claim. Many legal experts identify poor documentation (incomplete, inaccurate, or missing) as one of the most common nursing errors committed across the country and recommend that nurses make the effort to document each intervention they perform. In other words, “If it wasn’t written down, it never happened.”
In addition to legal liability, you also risk suspension or revocation of your license by your state’s board of nursing. The National Council for State Boards of Nursing, a nonprofit organization comprised of members from the boards of nursing in all 50 states, reports that cases of practice-related discipline commonly involve a breakdown or error in the nursing process, including failure to accurately document. NSO states: “While missing documentation can impede the ability to defend a nurse in a professional liability lawsuit, fraudulent or falsified documentation can also lead to a state board of nursing complaint.”
Investigations by a board of nursing vary by state, and depending on the severity of the allegation may require only a written statement from the nurse in response to the accusation or the board might decide to conduct a full investigation with witness interviews. This process can take several months. Once complete, the board will decide whether to close the case or file formal charges and present evidence at a hearing. Possible sanctions include fines, a reprimand or censure, probation, suspension, or revocation of your nursing license.
Statutes of limitation don’t apply to licensure revocation and disciplinary proceedings, so it might be several years before you’re notified of an allegation. Disciplinary actions are considered public information and are published in state and national databases, newsletters, websites, and Nursys, the national database for nurse licensure verification.
Address the challenges
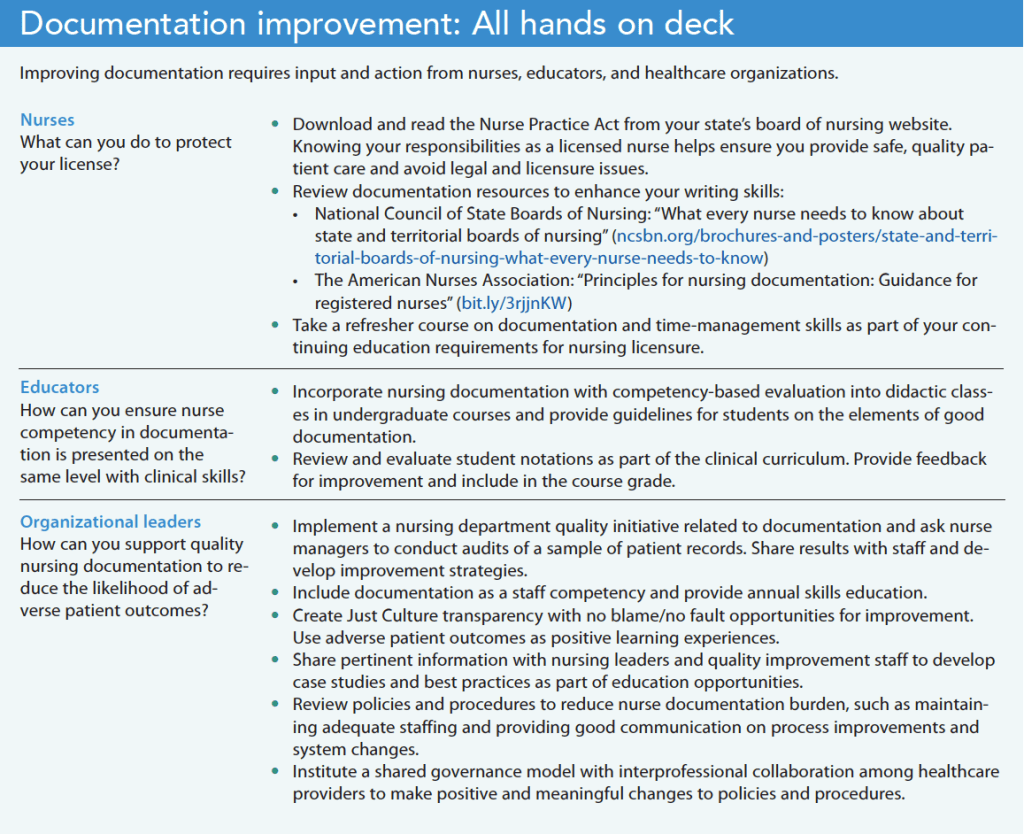
Complete and accurate documentation provides a clear picture of a patient’s condition and how they’re responding to treatment, which then influences providers’ care decisions. Nurses face many time constraints and interruptions throughout their shifts that make documentation difficult, but this essential care step is just as important as your clinical proficiency. Nurses, educators, and organizations can take steps to address documentation challenges and ensure excellent quality of care. (See Documentation improvement: All hands on deck .)
American Nurse Journal. 2023; 18(8). Doi: 10.51256/ANJ082328
American Nurses Association. Principles for Nursing Documentation: Guidance for Registered Nurses. 2010. nursingworld.org/~4af4f2/globalassets/docs/ana/ethics/principles-of-nursing-documentation.pdf
Gallegos A. Medscape malpractice report 2021. Medscape. November 19, 2021. medscape.com/slideshow/2021-malpractice-report-6014604#12
Iuppa N. Improving the electronic health record experience for nurses. Cleveland Clinic. consultqd.clevelandclinic.org/improving-the-electronic-health-record-experience-for-nurses
Leventhal R. Malpractice claims report: EHR documentation errors still far too common. Healthcare Innovation. November 4, 2020. hcinnovationgroup.com/clinical-it/electronic-health-record-electronic-medical-record-ehr-emr/news/21161325/malpractice-claims-report-ehr-documentation-errors-still-far-too-common
McKnight H, Moore SM. Nursing shared governance . Updated September 19, 2022. StatPearls. ncbi.nlm.nih.gov/books/NBK549862/
National Council for State Boards of Nursing. Discipline. ncsbn.org/discipline.htm
Nurses Service Organization and CNA. Nurse Professional liability exposure claim report: 4th edition: Minimizing risk, achieving excellence. 2020. nso.com/Learning/Artifacts/Claim-Reports/Minimizing-Risk-Achieving-Excellence
NurseJournal. The 5 most common mistakes made by new nurses. April 27, 2022. nursejournal.org/articles/most-common-mistakes-made-by-new-nurses
Nursing OnPoint. Nursing documentation. nursingonpoint.com/clinical-resources/documentation-laws-regulations/nursing-documentation/#2
Key words: nursing documentation, quality care, patient safety, nursing licensure
Let Us Know What You Think
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Centered on nurses
Innovations to keep patients and nurses safe

Simulation: Preparing for workplace violence

Anti-racism in nursing

Medication safety
Built to fit

ANA Enterprise News, October 2024

Responding to workplace violence

Answering the call

Creating an organization for future generations

Firearm safety: Nurses’ knowledge and comfort

The Secret Garden: A staff-only wellness and respite space
Healthy Nurse, Healthy Nation: 2024 Highlights Report
Nurses build coalitions at the Capitol


Stop fall prevention practices that aren’t working
Hankey L. Proper documentation protects patients and your license. American Nurse Journal. 2023;18(8):28-31. doi:10.51256/anj082328 https://www.myamericannurse.com/proper-documentation-protects-patients-and-your-license/
Career Advice > Professional Development > Upskilling and Promotions > Documentation for Nurses: Best Practices
Documentation for Nurses: Best Practices
Search resource center.

Raise your hand if you’ve ever heard, “If you didn’t document it, you didn’t do it.” If we had to boil down all of the best practices of documentation for nurses, this would be the golden rule.
What should you document? What is okay and what should be avoided? Why is nursing documentation so important? We’ll answer all of those questions and cover the do’s and don’ts of documentation in nursing in this article.
What Does Nursing Documentation Mean?
Nursing documentation refers to a nurse’s written or electronic additions to a patient’s chart. Practically every job you have will have its own set of required documentation for nurses, which will vary depending on the facility, role, and specialty.
For example, a nurse working in the intensive care unit (ICU) may be required to document physical assessments on all of their patients every four hours. A nurse working in the medical surgical unit may have this requirement once per shift.
What Is the Importance of Documentation in Nursing?
Nursing documentation is essential for communicating clinically relevant information to the healthcare team. It details nursing assessments and interventions, narrates changes in clinical status, states pertinent and relevant patient information, and provides evidence of care.
Many decisions are made based on nurses’ documentation. For example, a physician may review the nurse’s notes to evaluate medical interventions and the plan of care. A fellow nurse may compare previously charted nursing assessments with their current assessment in order to identify changes in patient status. These practices must also follow HIPAA guidelines to maintain patient privacy.
Documentation creates a record of services that is relied upon by payors (i.e. Medicare) for reimbursement of services . It may also be used as evidence in legal cases , reviewed for clinical research , and evaluated for quality assurance. Documentation is also often reviewed by certified clinical documentation specialists (CCDS), who verify the accuracy of information.
Timely Documentation in Nursing
While nurses typically have their entire shift to complete their documentation, it is encouraged to chart promptly. Remember, other healthcare members rely upon nursing notes . If a patient’s chart shows an elevated blood pressure, but the nurse has not made any notes addressing it, others may become concerned.
Additional charting requirements may arise depending on the patient’s status and diagnosis. If a patient received tPA , the nurse must perform (and document) neuro assessments every 15 minutes for the first two hours. Thus, nurses must be familiar with their facility policies as well as professional best practices regarding what type of documentation is required.
What Needs to Be Documented by a Nurse?
Simply put, everything a nurse does should be documented — from assessing a patient to calling the doctor to turning on a patient’s bed alarm. Examples of nurses’ documentation include:
- Patient head-to-toe assessments
- Change in clinical status
- Intervention and evaluation
- Patient and family education
Types of Documentation in Nursing
Most nursing documentation is implemented electronically in the patient’s electronic medical record (EMR), through programs like Epic charting . There are a few different formats and methods nurses follow when documenting, and some nurses use brain sheets to take notes on patients’ information. Common types include:
- Narrative documentation
- Progress note
- Charting by exception
- Situation, background, assessment, and recommendation (SBAR)
- Problem-focused documentation (i.e. SOAP)
Documentation for Nurses: Do’s and Don’ts
A nurse’s documentation becomes a part of a permanent record in the patient’s medical chart. Incomplete or improper charting can lead to serious medical errors and other consequences. You can help mitigate those potential outcomes by learning and following the best practices for documentation.
Do’s of Nursing Documentation
- Include objective statements.
- Use quotes.
- Describe findings.
- Document refusal of care.
- Include timestamps.
1. Include Objective Statements
Relay your assessment findings in your nurse’s notes. Stick to the data. Record vital signs, physical exam findings, intake and output, and other measurements. Learn more about the difference between subjective vs. objective nursing data .
Example: Patient’s blood pressure measures 125/58.
2. Use Quotes
There are moments when it is important to record exactly what words the patient said. To make it clear that it’s the patient’s actual words, and not the nurse’s interpretation, use quotation marks.
Example: The patient said, “I cannot take that medication. Last time it made me itchy all over my body and it was hard to breathe.”
3. Describe Findings
Paint a picture with your clinical findings. Do not just say that the patient has a wound — describe it. Where was it? How did it look? What were the measurements?
Example: Ecchymosis noted on torso, blue and green in color, measures 1 x 2 in.
4. Document Refusal of Care
There may be times when a patient refuses care, whether a bath or medication. It is their right as the patient to accept or deny care. As the nurse, your duty is to record this interaction along with any other relevant information.
Example: Patient refused to be repositioned at 1600. Patient states, “I am comfortable just like this. I’ll let you know when I need help turning.” Educated patient on the importance of repositioning and tissue integrity. Patient verbalized understanding.
5. Include Timestamps
Timely documentation in nursing is pivotal. While the EMR will automatically timestamp documentation for nurses, it will do so for each entry, not when the event actually occurred. When making a nurse’s note, be sure to clearly convey the time symptoms appeared, when the doctor was called, when an intervention was implemented, and when the patient was reassessed.
- 0900 Patient reported pain of 6/10 to their right shoulder.
- 0910 Pain medication given, see MAR.
- 0945 Patient reassessed, reports pain has reduced to 3/10. Patient repositioned. Will continue to monitor.
Don’ts of Nursing Documentation
- Don’t use subjective descriptions.
- Don’t label patients.
- Don’t chart for others.
- Don’t document preemptively.
- Don’t use improper medical abbreviations.
1. Don’t Use Subjective Descriptions
You don’t need to add your opinion or feelings about a patient’s status. When it comes to documentation for nurses, stick to the facts and let the numbers speak for themselves. Avoid vague terms like: large, bad, worse, small, less, little, and better.
Example: Patient’s O2 sat dropped very low.
2. Don’t Label Patients
Similarly, do not document your opinion, assumptions, or feelings of a patient. Describe their presentation, clinical findings, behavior, and gestures. When necessary, document quotations of their statements.
Example: Patient is a frequent flier and drug seeker who presented to the ER saying nonsensical things.
3. Don’t Chart for Others
Only chart what you have done and what you have observed. This means that you should not chart findings based on what you have been told — chart what you have found, assessed, and measured.
When you make a nurse’s note, you are attaching your name to it. Clearly stating who rendered care is of utmost importance in clinical documentation in nursing. Keep in mind that nurses’ documentation can include the name of another nurse who assisted in the patient’s care when necessary.
4. Don’t Document Preemptively
While it can be tempting to save time, only document things you’ve actually done or assessed.
Things can change in an instant. You may plan to give Tylenol to the patient in room 40, but until it’s been given, do not document it. You never know whether a patient will refuse a medication, spit it out, experience a decline in health, or have their orders changed.
5. Don’t Use Improper Medical Abbreviations
There are many, many abbreviations in medical terminology. Stick to universally accepted ones to avoid potential misunderstanding and subsequent errors. Refer to this “Do Not Use” list for terms to avoid.
Example: Patient received 2u blood. (Instead of “u,” spell out “units.”)
Put These Tips Into Practice
Using these best practices in documentation for nurses can help you become a better nurse. Looking for somewhere new to use these skills? IntelyCare can match you with nurse jobs in your desired facility type and specialty. Get started today.
Related Articles
Networking in nursing: 10 tips to get connected, who is imogene king nursing theory explainer, guide to martha rogers’ nursing theory, 5 tips to write a personal philosophy of nursing, 13 halloween costumes for nurses at work, related jobs.

IMAGES
VIDEO