An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.


Endotext [Internet].
- www.endotext.org
Definitions, Classification, and Epidemiology of Obesity
Jonathan Q. Purnell , MD.
Last Update: May 4, 2023 .
Recent research has established the physiology of weight regulation, the pathophysiology that leads to unwanted weight gain with establishment of a higher body-weight set point, and the defense of the overweight and obese state even when reasonable attempts in lifestyle improvement are made. This knowledge has informed our approach to obesity as a chronic disease. The assessment of adiposity risk for the foreseeable future will continue to rely on cost-effective and easily available measures of height, weight, and waist circumference. This risk assessment then informs implementation of appropriate treatment plans and weight management goals. Within the United States, prevalence rates for generalized obesity (BMI > 30 kg/m 2 ), extreme obesity (BMI > 40 kg/m 2 ), and central obesity continue to rise in children and adults with peak obesity rates occurring in the 5 th -6 th decades. Women may have equal or greater obesity rates than men depending on race, but less central obesity than men. Obesity disproportionately affects people by race and ethnicity, with the highest prevalence rates reported in Black women and Hispanic men and women. Increasing obesity rates in youth (ages 2-19 years) are especially concerning. This trend will likely continue to fuel the global obesity epidemic for decades to come, worsening population health, creating infrastructural challenges as countries attempt to meet the additional health-care demands, and greatly increasing health-care expenditures world-wide. To meet this challenge, societal and economic innovations will be necessary that focus on strategies to prevent further increases in overweight and obesity rates. For complete coverage of all related areas of Endocrinology, please visit our on-line FREE web-text, WWW.ENDOTEXT.ORG .
- INTRODUCTION
Unwanted weight gain leading to overweight and obesity has become a significant driver of the global rise in chronic, non-communicable diseases and is itself now considered a chronic disease. Because of the psychological and social stigmata that accompany developing overweight and obesity, those affected by these conditions are also vulnerable to discrimination in their personal and work lives, low self-esteem, and depression ( 1 ). These medical and psychological sequelae of obesity contribute to a major share of health-care expenditures and generate additional economic costs through loss of worker productivity, increased disability, and premature loss of life ( 2 - 4 ).
The recognition that being overweight or having obesity is a chronic disease and not simply due to poor self-control or a lack of will power comes from the past 70 years of research that has been steadily gaining insight into the physiology that governs body weight (homeostatic mechanisms involved in sensing and adapting to changes in the body’s internal metabolism, food availability, and activity levels so as to maintain fat content and body weight stability), the pathophysiology that leads to unwanted weight gain maintenance, and the roles that excess weight and fat maldistribution (adiposity) play in contributing to diabetes, dyslipidemia, heart disease, non-alcoholic fatty liver disease, obstructive sleep apnea, and many other chronic diseases ( 5 , 6 ).
Expression of overweight and obesity results from an interaction between an individual’s genetic predisposition to weight gain and environmental influences. Gene discovery in the field of weight regulation and obesity has identified several major monogenic defects resulting in hyperphagia accompanied by severe and early-onset obesity ( 7 ) as well as many more minor genes with more variable impact on weight and fat distribution, including age-of-onset and severity. Several of these major obesity genes now have a specific medication approved to treat affected individuals ( 8 ). However, currently known major and minor genes explain only a small portion of body weight variations in the population ( 7 ). Environmental contributors to obesity have also been identified ( 9 ) but countering these will likely require initiatives that fall far outside of the discussions taking place in the office setting between patient and provider since they involve making major societal changes regarding food quality and availability, work-related and leisure-time activities, and social and health determinants including disparities in socio-economic status, race, and gender.
Novel discoveries in the fields of neuroendocrine ( 6 ) and gastrointestinal control ( 10 ) of appetite and energy expenditure have led to an emerging portfolio of medications that, when added to behavioral and lifestyle improvements, can help restore appetite control and allow modest weight loss maintenance ( 8 ). They have also led to novel mechanisms that help to explain the superior outcomes, both in terms of meaningful and sustained weight loss as well as improvements or resolution of co-morbid conditions, following metabolic-bariatric procedures such as laparoscopic sleeve gastrectomy and gastric bypass ( 11 , 12 ).
Subsequent chapters in this section of Endotext will delve more deeply into these determinants and scientific advances, providing a greater breadth of information regarding mechanisms, clinical manifestations, treatment options, and prevention strategies for those with overweight or obesity.
- DEFINITION OF OVERWEIGHT AND OBESITY
Overweight and obesity occur when excess fat accumulation (globally, regionally, and in organs as ectopic lipids) increases risk for adverse health outcomes . Like other chronic diseases, this definition does not require manifistation of an obesity-related complication, simply that the risk for one is increased. This allows for implementation of weight management strategies targeting treatment and prevention of these related conditions. It is important to point out that thresholds of excess adiposity can occur at different body weights and fat distributions depending on the person or population being referenced.
Ideally, an obesity classification system would be based on a practical measurement widely available to providers regardless of their setting, would accurately predict health risk (prognosis), and could be used to assign treatment stategies and goals. The most accurate measures of body fat adiposity such as underwater weighing, dual-energy x-ray absorptiometry (DEXA) scanning, computed tomograpy (CT), and magnetic resonance imaging (MRI) are impractical for use in everyday clinical encounters. Estimates of body fat, including body mass index (BMI, calculated by dividing the body weight in kilograms by height in meters squared) and waist circumference, have limitations compared to these imaging methods, but still provide relevant information and are easily obtained in a variety of practice settings.
It is worth pointing out two important caveats regarding cuurent thresholds used to diagnose overweight and obesity. The first is that although we favor the assignement of specific BMI cut-offs and increasing risk ( Table 1 ), relationships between body weight or fat distribution and conditions that impair health actually represent a continum. For example, increased risk for type 2 diabetes and premature mortality occur well below a BMI of 30 kg/m 2 (the threshold to define obesity in populations of European extraction) ( 13 ). It is in these earlier stages that preventative strategies to limit further weight gain and/or allow weight loss will have their greatest health benefits. The second is that historic relationships between increasing BMI thresholds and the precense and severity of co-morbidities have been disrupted as better treatments for obesity-complications become available. For example, in the past several decades, atherosclerotic cardiovascular (ASCVD) mortality has steadily declined in the US population ( 14 ) even as obesity rates have risen (see below). Although it is generally accepted that this decline in ASCVD deaths is due to better care outside the hospital during a coronary event (e.g., better coordination of “first responders” services such as ambulances and more widespread use by the public of cardiopulmonary resusitation and defibrillator units), advances in intensive care, smoking cessation, and in the office (increased use of aspirin, statins, PCSK9 inhibitors, and blood pressure medications) ( 15 ), these data have also been cited to support the claim that being overweight might actually protect against heart disease ( 16 ). In this regard, updated epidemiological data on the health outcomes related to being overweight or having obesity should include not just data on morbidity and mortality, but also health care metrics such as utilization and costs, medications used, and the number of treatment-related procedures performed.
- CLASSIFICATION OF OVERWEIGHT, OBESITY, AND CENTRAL OBESITY
Fat Mass and Percent Body Fat
Fat mass can be directly measured by one of several imaging modalities, including DEXA, CT, and MRI, but these systems are impractical and cost prohibitive for general clinical use. Instead, they are mostly used for research. Fat mass can be measured indirectly using water (underwater weighing) or air displacement (BODPOD), or bioimpedance analysis (BIA). Each of these methods estimates the proportion of fat or non-fat mass and allows calcutation of percent body fat. Of these, BODPOD and BIA are often offered through fitness centers and clinics run by obesity medicine specialists. However, their general use in the care of patients who are overweight and with obesity is still limited. Interpretation of results from these procedures may be confounded by common conditions that accompany obesity, especially when fluid status is altered such as in congenstive heart failure, liver disease, or chronic kidney disease. Also, ranges for normal and abnormal are not well established for these methods and, in practical terms, knowing them will not change current recommendations to help patients achieve sustained weight loss.
Body Mass Index
Body mass index allows comparison of weights independently of stature across populations. Except in persons who have increased lean weight as a result of intense exercise or resistance training (e.g., bodybuilders), BMI correlates well with percentage of body fat, although this relationship is independently influenced by sex, age, and race ( 17 ). This is especially true for South Asians in whom evidence suggests that BMI-adjusted percent body fat is greater than other populations ( 18 ). In the United States, data from the second National Health and Nutrition Examination Survey (NHANES II) were used to define obesity in adults as a BMI of 27.3 kg/m 2 or more for women and a BMI of 27.8 kg/m 2 or more for men ( 19 ). These definitions were based on the gender-specific 85 th percentile values of BMI for persons 20 to 29 years of age. In 1998, however, the National Institutes of Health (NIH) Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults adopted the World Health Organization (WHO) classification for overweight and obesity ( Table 1 ) ( 20 ). The WHO classification, which predominantly applied to people of European ancestry, assigns increasing risk for comorbid conditions—including hypertension, type 2 diabetes mellitus, and cardiovascular disease—to persons with higher a BMI relative to persons of normal weight (BMI of 18.5 - 25 kg/m 2 ) ( Table 1 ). However, Asian populations are known to be at increased risk for diabetes and hypertension at lower BMI ranges than those for non-Asian groups due largely to predominance of central fat distribution and higer percentage fat mass (see below). Consequently, the WHO has suggested lower cutoff points for consideration of therapeutic intervention in Asians: a BMI of 18.5 to 23 kg/m 2 represents acceptable risk, 23 to 27.5 kg/m 2 confers increased risk, and 27.5 kg/m 2 or higher represents high risk ( 21 , 22 ).
Classification of Overweight and Obesity by BMI, Waist Circumference, and Associated Disease Risk. Adapted from reference ( 20 ).
View in own window
Disease risk for type 2 diabetes, hypertension, and cardiovascular disease.
Increased waist circumference can also be a marker for increased risk even in persons of normal weight.
Fat Distribution (Central Obesity)
In addition to an increase in total body weight, a proportionally greater amount of fat in the abdomen or trunk compared with the hips and lower extremities has been associated with increased risk for metabolic syndrome, type 2 diabetes mellitus, hypertension, and heart disease in both men and women ( 23 , 24 ). Abdominal obesity is commonly reported as a waist-to-hip ratio, but it is most easily quantified by a single circumferential measurement obtained at the level of the superior iliac crest ( 20 ). For the practioner, waist circumference should be measured in a standardized way ( 20 ) at each patient’s visit along with body weight. The original US national guidelines on overweight and obesity categorized men at increased relative risk for co-morbidities such as diabetes and cardiovascular disease if they have a waist circumference greater than 102 cm (40 inches) and women if their waist circumference exceeds 88 cm (35 inches) ( Table 1 ) ( 20 ). These waist circumference thresholds are also used to define the “metabolic syndrome” by the most recent guidelines from the American Heart Association and the National Lipid Association (e.g., triglyceride levels > 150 mg/dL, hypertension, elevated fasting glucose (100 – 125 mg/dL)) or prediabetes (hemoglobin A1c between 5.7 and 6.4%) ( 25 , 26 ). Thus, an overweight person with predominantly abdominal fat accumulation would be considered “high” risk for these diseases even if that person does not meet BMI criteria for obesity. Such persons would have “central obesity.” It is commonly accepted that the predictive value for increased health risk by waist circumference is in patients at lower BMI’s (< 35 kg/m 2 ) since those with class 2 obesity or higher will nearly universally have waist circumferences that exceed disease risk cut-offs.
However, the relationships between central adiposity with co-morbidities are also a continuum and vary by race and ethnicity. For example, in those of Asian descent, abdominal (central) obesity has long been recognized to be a better disease risk predictor than BMI, especially for type 2 diabetes ( 27 ). As endorsed by the International Diabetes Federation ( 28 ) and summarized in a WHO report in 2008 ( 29 ), different countries and health organizations have adopted differing sex- and population-specific cut offs for waist circumference thresholds predictive of increased comorbidity risk. In addition to the US criteria, alternative thresholds for central obesity as measured by waist circumference include > 94 cm (37 inches) and > 80 cm (31.5 inches) for men and women of European anscestry and > 90 cm (35.5 inches) and > 80 cm (31.5 inches) for men and women of South Asian, Japanese, and Chinese origin ( 28 , 29 ), respectively.
- EPIDEMIOLOGY OF OVERWEIGHT AND OBESITY IN THE UNITED STATES
In the United States (US), data from the National Health and Nutrition Examination Survey using measured heights and weights shows that the steady increase in obesity prevalence in both children and adults over the past several decades has not waned, although there are exceptions among subpopulations as described in greater detail below. In the most recently published US report (2017-2020), 42.4% of adults (BMI ≥ 30 kg/m 2 ) ( 30 ) and 20.9% of youth (BMI ≥ 95 th percentile of age- and sex-specific growth charts) ( 31 ) have obesity, and the age-adjusted prevalence of severe obesity (BMI ≥ 40 kg/m 2 ) was 9.2% ( 30 ) ( Figure 1 ).

Trends in age-adjusted obesity (BMI ≥ 30 kg/m 2 ) and severe obesity (BMI ≥ 40 kg/m 2 ) prevalence among adults aged 20 and over: United States, 1999–2000 through 2017–2018. Taken from reference ( 30 ).
Obesity and Severe Obesity in Adults: Relationships with Age, Sex, and Demographics

Age-Adjusted Prevalence of Obesity and Severe Obesity in US Adults. National Health and Nutrition Examination Survey data, prevalence estimates are weighted and age-adjusted to the projected 2000 Census population using age groups 20-39, 40-59, and 60 or older. Significant linear trends (P < .001) for all groups except for obesity among non-Hispanic Black men, which increased from 1999-2000 to 2005-2006 and then leveled after 2005-2006. Data taken from reference ( 31 ).
On average, the obesity rate in US adults has nearly tripled since the 1960’s (Reference ( 32 ) and Figure 2 ). These large increases in the number of people with obesity and severe obesity, while at the same time the level of overweight has remained steady ( 32 , 33 ), suggests that the “obesogenic” environment is disproportionately affecting those portions of the population with the greatest genetic potential for weight gain ( 34 ). This currently leaves slightly less than 30% of the US adult population as having a healthy weight (BMI between 18.5 and 25 kg/m 2 ).
Men and women now have similar rates of obesity and the peak rates of obesity for both men and women in the US occur between the ages of 40 and 60 years ( Figures 2 and 3 ). In studies that have measured body composition, fat mass also peaks just past middle age in both men and women, but percent body fat continues to increase past this age, particularly in men because of a proportionally greater loss in lean mass ( 35 - 37 ). The menopausal period has also been associated with an increase in percent body fat and propensity for central (visceral) fat distribution, even though total body weight may change very little during this time ( 38 - 41 ).
The rise in obesity prevalence rates has disproportionately affected US minority populations ( Figure 2 ). The highest prevelance rates of obesity by race and ethnicity are currently reported in Black women, native americans, and Hispanics ( Figure 2 and reference ( 42 )). In general, women and men who did not go to college were more likely to have obesity than those who did, but for both groups these relationships varied depending on race and ethnicity (see below). Amongst women, obesity prevelance rates decreased with increasing income in women (from 45.2% to 29.7%), but there was no difference in obesity prevalence between the lowest (31.5%) and highest (32.6%) income groups among men ( 43 ).

Prevalence of obesity among adults aged 20 and over, by sex and age: United States, 2017–2018. Taken from reference ( 30 ).
The interactions of socieconomic status and obesity rates varied based on race and ethnicity ( 43 ). For example, the expected inverse relationship between obesity and income group did not hold for non-Hispanic Black men and women in whom obesity prevelance was actually higher in the highest compared to lowest income group (men) or showed no relationship to income by racial group at all (women) ( 43 ). Obesity prevalence was lower among college graduates than among persons with less education for non-Hispanic White women and men, Black women, and Hispanic women, but not for Black and Hispanic men. Asian men and women have the lowest obesity prevelance rates, which did not vary by eduction or income level ( 43 ).
Central Obesity
As discussed above, central weight distribution occurs more commonly in men than women and increases in both men and women with age. In one of the few datasets that have published time-trends in waist circumference, it has been shown that over the past 20 years, age-adjusted waist circumferences have tracked upward in both US men and women ( Figure 4 ). Much of this likely reflects the population increases in obesity prevelance since increasing fat mass and visceral fat track together ( 52 ).

Age-adjusted mean waist circumference among adults in the National Health and Nutrition Examination Survey 1999-2012. Adapted from ( 51 ).
Childhood obesity is a risk factor for adulthood obesity ( 44 - 46 ). In this regard, the similar tripling of obesity rates in US youth (ages 2-19 years old) ( Figure 5 ) to 20.9% in 2018 ( 31 ) is worrisome and will contribute to the already dismal projections of the US adult population approaching 50% obesity prevelance by the year 2030 ( 47 ). Obesity prevalence was 26.2% among Hispanic children, 24.8% among non-Hispanic Black children, 16.6% among non-Hispanic White children, and 9.0% among non-Hispanic Asian children ( 48 ). Like adults, obesity rates in children are greater when they are live in households with lower incomes and less education of the head of the household ( 49 ). In this regard, these obesity gaps have been steadily widening in girls, whereas the differences between boys has been relatively stable ( 49 ).

Trends in obesity among children and adolescents aged 2–19 years, by age: United States, 1963–1965 through 2017–2018. Obesity is defined as body mass index (BMI) greater than or equal to the 95th percentile from the sex-specific BMI-for-age 2000 CDC Growth Charts. Taken from reference ( 50 ).
With regard to socieconomic status, the inverse trends for lower obesity rates and higher income and education (of households) held in all race and ethnic origin groups with the following exceptions: obesity prevalence was lower in the highest income group only in Hispanic and Asian boys and did not differ by income among non-Hispanic Black girls ( 49 ).
- INTERNATIONAL TRENDS IN OBESITY
Historically, international obesity rates have been lower than in the US, and most developing countries considered undernutrition to be their topmost health priority ( 53 ). However, international rates of overweight and obesity have been rising steadily for the past several decades and, in many countries, are now meeting or exceeding those of the US ( Figure 6 ) ( 54 , 55 ). In 2016, 1.3 billion adults were overweight worldwide and, between 1975 to 2016, the number of adults with obesity increased over six-fold, from 100 million to 671 million (69 to 390 million women, 31 to 281 million men) ( 54 ). Especially worrisome have been similar trends in the youth around the world ( Figure 6 ), from 5 million girls and 6 million boys with obesity in 1975 to 50 million girls and 74 million boys in 2016 ( 54 ), as this means the rise in obesity rates will continue for decades as they mature into adults.
The growth in the wordwide prelance of overweight and obesity is thought to be primarily driven by economic and technological advancements in all developing societies ( 56 , 57 ). These forces have been ongoing in the US and other Western countries for many decards but are being experienced by many developing countries on a compressed timescale. Greater worker productivity in advancing economies means more time spent in sedentary work (less in manual labor) and less time spent in leisure activity. Greater wealth allows the purchase of televisions, cars, processed foods, and more meals eaten out of the house, all of which have been associated with greater rates of obesity in children and adults. More details and greater discussion of these issues can be found in Endotext Chapters on Non-excercise Activity Thermogenesis ( 58 ) and Obesity and the Environment ( 9 ).
Regardless of the causes, these trends in global weight gain and obesity are quickly creating a tremendous burden on health-care systems and cost to countries attempting to respond to the increased treatment demands ( 59 ). They are also feuling a rise in global morbity and mortality for chronic (non-communicable) diseases, especially for cardiovascular disease and type 2 diabetes mellitus, and especially in Asian and South Asian populations where rates of type 2 diabetes are currently exploding ( 15 , 60 - 63 ). Efforts need to be made to deliver adequate health care to those currently with obesity and, at the same time, find innovative and alternative solutions that allow economies to prosper and to incorporate technologies that will reverse current trends in obesity and obesity-related complications.
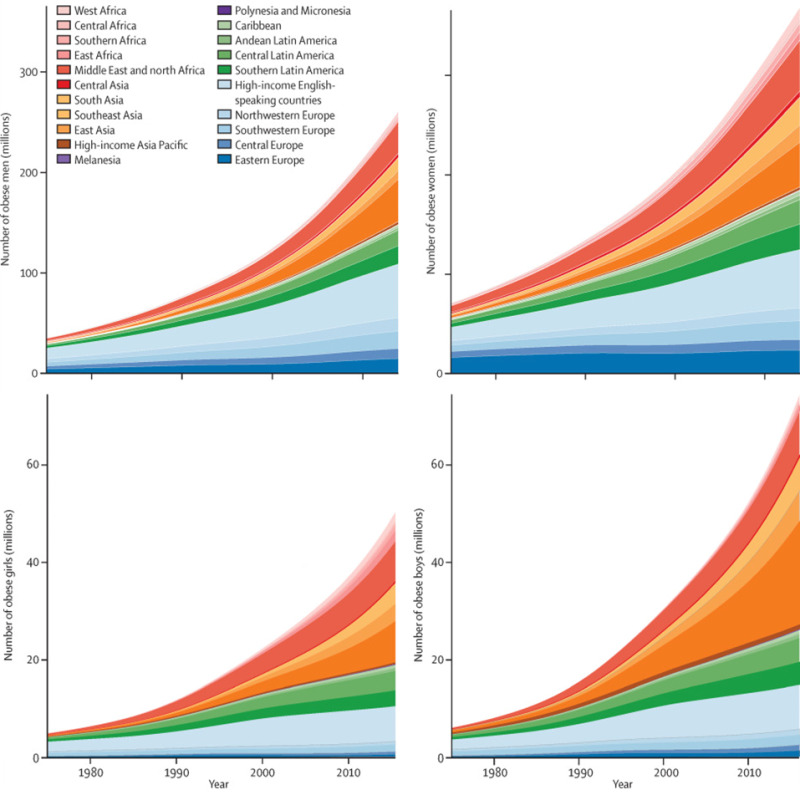
Trends in the number of adults, children, and adolescents with obesity and with moderate and severe underweight by region. Children and adolescents were aged 5–19 years. (Taken from ( 54 )).
Obesity is both a chronic disease in its own right and a primary contributor to other leading chronic diseases such as type 2 diabetes, dyslipidemia, hypertension, and cardiovascular diseases. In the clinic, obesity is still best defined using commonly available tools, including BMI and waist circumference; although it is hoped that newer imaging modalities allowing more precise quantification of amount and distribution of excess lipid depots will improve obesity risk assessment. The general rise in obesity taking place in the US over the past 50 years is now occurring globally. In the US, the prevalence rates of obesity in adult men and women are now similar at 40%, and minorities are disproportionately affected, including Blacks, Native Americans, and Hispanics, with obesity rates of 50% or higher. Particularly worrisome is the global increase in obesity prevalence in children and adolescents as these groups will continue to contribute to a rising adult obesity rates for several decades to come. As important as finding solutions that address the global logistical and financial challenges facing health-care systems attempting to meet current demands of obesity and weight-related co-morbidities will be finding innovative solutions that prevent and reverse current population weight gain trends.
This electronic version has been made freely available under a Creative Commons (CC-BY-NC-ND) license. A copy of the license can be viewed at http://creativecommons.org/licenses/by-nc-nd/2.0/ .
- Cite this Page Purnell JQ. Definitions, Classification, and Epidemiology of Obesity. [Updated 2023 May 4]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
In this Page
Links to www.endotext.org.
- View this chapter in Endotext.org
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- The effectiveness of web-based programs on the reduction of childhood obesity in school-aged children: A systematic review. [JBI Libr Syst Rev. 2012] The effectiveness of web-based programs on the reduction of childhood obesity in school-aged children: A systematic review. Antwi F, Fazylova N, Garcon MC, Lopez L, Rubiano R, Slyer JT. JBI Libr Syst Rev. 2012; 10(42 Suppl):1-14.
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. [Cochrane Database Syst Rev. 2022] Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, et al. Cochrane Database Syst Rev. 2022 Feb 1; 2(2022). Epub 2022 Feb 1.
- Review Screening and Interventions for Childhood Overweight [ 2005] Review Screening and Interventions for Childhood Overweight Whitlock EP, Williams SB, Gold R, Smith P, Shipman S. 2005 Jul
- Review Body Weight Regulation. [Endotext. 2000] Review Body Weight Regulation. Woolf EK, Cabre HE, Niclou AN, Redman LM. Endotext. 2000
- Trends in Adiposity and Food Insecurity Among US Adults. [JAMA Netw Open. 2020] Trends in Adiposity and Food Insecurity Among US Adults. Myers CA, Mire EF, Katzmarzyk PT. JAMA Netw Open. 2020 Aug 3; 3(8):e2012767. Epub 2020 Aug 3.
Recent Activity
- Definitions, Classification, and Epidemiology of Obesity - Endotext Definitions, Classification, and Epidemiology of Obesity - Endotext
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- For educators
- English (US)
- English (India)
- English (UK)
- Greek Alphabet
This problem has been solved!
You'll get a detailed solution from a subject matter expert that helps you learn core concepts.
Question: Research studies on obesity and healthcare have found that _________.Most nurses understand that obesity can be easily prevented by self-control.Overweight people are less likely to receive preventive care than others.Medical professionals do not hold the same negative perceptions that employers hold about those who are overweight.The attitude of medical
Research studies on obesity and healthcare have found that ____:
This is an incomplete statement, and...
Not the question you’re looking for?
Post any question and get expert help quickly.
- Open access
- Published: 15 August 2018
How and why weight stigma drives the obesity ‘epidemic’ and harms health
- A. Janet Tomiyama 1 ,
- Deborah Carr 2 ,
- Ellen M. Granberg 3 ,
- Brenda Major 4 ,
- Eric Robinson 5 ,
- Angelina R. Sutin 6 &
- Alexandra Brewis 7
BMC Medicine volume 16 , Article number: 123 ( 2018 ) Cite this article
150k Accesses
377 Citations
1605 Altmetric
Metrics details
In an era when obesity prevalence is high throughout much of the world, there is a correspondingly pervasive and strong culture of weight stigma. For example, representative studies show that some forms of weight discrimination are more prevalent even than discrimination based on race or ethnicity.
In this Opinion article, we review compelling evidence that weight stigma is harmful to health, over and above objective body mass index. Weight stigma is prospectively related to heightened mortality and other chronic diseases and conditions. Most ironically, it actually begets heightened risk of obesity through multiple obesogenic pathways. Weight stigma is particularly prevalent and detrimental in healthcare settings, with documented high levels of ‘anti-fat’ bias in healthcare providers, patients with obesity receiving poorer care and having worse outcomes, and medical students with obesity reporting high levels of alcohol and substance use to cope with internalized weight stigma. In terms of solutions, the most effective and ethical approaches should be aimed at changing the behaviors and attitudes of those who stigmatize, rather than towards the targets of weight stigma. Medical training must address weight bias, training healthcare professionals about how it is perpetuated and on its potentially harmful effects on their patients.
Weight stigma is likely to drive weight gain and poor health and thus should be eradicated. This effort can begin by training compassionate and knowledgeable healthcare providers who will deliver better care and ultimately lessen the negative effects of weight stigma.
Peer Review reports
In a classic study performed in the late 1950s, 10- and 11-year-olds were shown six images of children and asked to rank them in the order of which child they ‘liked best’. The six images included a ‘normal’ weight child, an ‘obese’ child, a child in a wheelchair, one with crutches and a leg brace, one with a missing hand, and another with a facial disfigurement. Across six samples of varying social, economic, and racial/ethnic backgrounds from across the United States, the child with obesity was ranked last [ 1 ].
In the decades since, body weight stigma has spread and deepened globally [ 2 , 3 ]. We define weight stigma as the social rejection and devaluation that accrues to those who do not comply with prevailing social norms of adequate body weight and shape. This stigma is pervasive [ 4 , 5 , 6 ]; for example, in the United States, people with greater body mass index (BMI) report higher rates of discrimination because of their weight compared to reports of racial discrimination of ethnic minorities in some domains [ 7 ]. Women are particularly stigmatized due to their weight across multiple sectors, including employment, education, media, and romantic relationships, among others [ 8 ]. Importantly, weight stigma is also pervasive in healthcare settings [ 9 ], and has been observed among physicians, nurses, medical students, and dietitians [ 4 ]. Herein, we first address the obesogenic and health-harming nature of weight stigma, and then provide a discussion of weight stigma specifically in healthcare settings. We conclude with potential strategies to help eradicate weight stigma.
Weight stigma triggers obesogenic processes
Common wisdom and certain medical ethicists [ 10 , 11 ] assert that stigmatizing higher-weight individuals and applying social pressure to incite weight loss improves population health. We argue the opposite. The latest science indicates that weight stigma can trigger physiological and behavioral changes linked to poor metabolic health and increased weight gain [ 4 , 5 , 12 , 13 , 14 ]. In laboratory experiments, when study participants are manipulated to experience weight stigma, their eating increases [ 15 , 16 ], their self-regulation decreases [ 15 ], and their cortisol (an obesogenic hormone) levels are higher relative to controls, particularly among those who are or perceive themselves to be overweight. Additionally, survey data reveal that experiences with weight stigma correlate with avoidance of exercise [ 17 ]. The long-term consequences of weight stigma for weight gain, as this experimental and survey work suggests, have also been found in large longitudinal studies of adults and children, wherein self-reported experiences with weight stigma predict future weight gain and risk of having an ‘obese’ BMI, independent of baseline BMI [ 18 , 19 , 20 ].
The harmful effects of weight stigma may even extend to all-cause mortality. Across both the nationally representative Health and Retirement Study including 13,692 older adults and the Midlife in the United States (MIDUS) study including 5079 adults, people who reported experiencing weight discrimination had a 60% increased risk of dying, independent of BMI [ 21 ]. The underlying mechanisms explaining this relationship, which controls for BMI, may reflect the direct and indirect effects of chronic social stress. Biological pathways include dysregulation in metabolic health and inflammation, such as higher C-reactive protein, among individuals who experience weight discrimination [ 22 ]. In MIDUS and other studies, weight discrimination also amplified the relationship between abdominal obesity and HbA1c, and metabolic syndrome more generally [ 23 , 24 ]. Longitudinal data from MIDUS also showed that weight discrimination exacerbated the effects of obesity on self-reported functional mobility, perhaps because weight discrimination undermines one’s self-concept as a fully functioning, able person [ 25 ].
Weight stigma also has profound negative effects on mental health; nationally representative data from the United States show that individuals who perceive that they have been discriminated against on the basis of weight are roughly 2.5 times as likely to experience mood or anxiety disorders as those that do not, accounting for standard risk factors for mental illness and objective BMI [ 26 ]. Furthermore, this detrimental effect of weight stigma on mental health is not limited to the United States; weight-related rejection has also been shown to predict higher depression risk in other countries [ 27 ]. Importantly, the evidence indicates that the association generally runs from discrimination to poor mental health, rather than vice versa [ 27 ].
A rapidly growing set of studies now shows that these associations cannot simply be explained by higher-weight individuals’ poorer health or greater likelihood of perceiving weight-related discrimination. In fact, the mere perception of oneself as being overweight, across the BMI spectrum (i.e., even among individuals at a ‘normal’ BMI), is prospectively associated with biological markers of poorer health, including unhealthy blood pressure, C-reactive protein, HDL cholesterol, triglycerides, glucose, and HbA1c levels [ 28 ]. Emerging evidence indicates that this harmful cycle may even be intergenerational, wherein children perceived as overweight by their parents are at greater risk for excess weight gain across childhood [ 29 ], independent of the child’s actual weight. Collectively, these findings suggest that stigma attached to being ‘overweight’ is a significant yet unrecognized agent in the causal pathway from weight status to health.
Weight stigma in healthcare
Healthcare is a setting in which weight stigma is particularly pervasive, with significant consequences for the health of higher-weight patients [ 30 , 31 ]. A sample of 2284 physicians showed strong explicit and implicit ‘anti-fat’ bias [ 32 ]. High levels of bias are observed even among clinicians specializing in obesity-related issues, with the proportion endorsing explicit ‘anti-fat’ bias sentiments (e.g., ‘Fat people are worthless’) increasing in recent years [ 33 ]. The nature of healthcare provider bias encompasses endorsement of negative stereotypes of patients with obesity, including terms like ‘lazy’, ‘weak-willed’, and ‘bad’, feeling less respect for those patients, and being more likely to report them as a ‘waste of time’ [ 30 ].
This stigma has direct and observable consequences for the quality and nature of services provided to those with obesity, leading to yet another potential pathway through which weight stigma may contribute to higher rates of poor health. In terms of quality of care and medical decision-making, despite the fact that higher-weight patients are at elevated risk for endometrial and ovarian cancer, some physicians report a reluctance to perform pelvic exams [ 34 ] and higher-weight patients (despite having health insurance) delay having them [ 35 ]. Higher BMI male patients report that physicians spend less time with them compared to the time they spend with lower BMI patients [ 36 ]. Additionally, physicians engage in less health education with higher BMI patients [ 37 ].
In terms of quality of communication, higher-weight patients are clearly receiving the message that they are unwelcome or devalued in the clinical setting, frequently reporting feeling ignored and mistreated in clinical settings, and higher BMI adults are nearly three times as likely as persons with ‘normal’ BMI to say that they have been denied appropriate medical care [ 38 ]. Further, obese patients feel that their clinicians would prefer not to treat them [ 36 ]. As a result, patients with higher BMI report avoiding seeking healthcare because of the discomfort of being stigmatized [ 35 , 39 , 40 ]. Even when they do seek medical care, weight loss attempts are less successful when patients perceive that their primary care providers judge them on the basis of their weight [ 41 ].
Medical professionals are also not immune to experiencing weight bias. Medical students with a higher BMI report that clinical work can be particularly challenging, and those with a higher BMI who internalize ‘anti-fat’ attitudes also report more depressive symptoms and alcohol or substance abuse [ 42 ].
Tackling weight stigma
Many common anti-obesity efforts are unintentionally complicit in contributing to weight stigma. Standard medical advice for weight loss focuses on taking individual responsibility and exerting willpower (‘eat less, exercise more’). In this context, a little shame is seen as motivation to change diet and activity behaviors [ 10 , 11 ]. Nevertheless, this approach perpetuates stigmatization, as higher-weight individuals already engage in self-blame [ 43 ] and feel ashamed of their weight [ 44 ]. Stigma, therefore, maybe be an unintended consequence of anti-obesity efforts, undermining their intended effect. Moreover, focusing solely on obesity treatment runs the risk of missing other diagnoses, as was recently illustrated by Rebecca Hiles, whose multiple physicians failed to diagnose her lung cancer and instead repeatedly told her to lose weight in order to address her shortness of breath [ 45 ].
Traditional approaches to combatting obesity and poor metabolic health are clearly not working. Obesity rates remain high globally in both adults [ 46 , 47 ] and children [ 48 ], and even in those countries where rates appear to be plateauing, disparities continue to grow between dominant and minority groups (e.g., racial/ethnic minorities, lower socioeconomic status populations, and those with the highest BMI) [ 49 , 50 , 51 ]. Moreover, given the link between obesity, metabolic health, and stigma, the need to eradicate weight stigma is urgent. Metabolic diseases such as type II diabetes are at unprecedented levels in adults and children [ 52 ]. Governments and clinicians alike have struggled to find effective strategies to prevent weight gain, support weight loss, and promote metabolic health. The science of weight stigma crystallizes a key point for future success – to tackle the obesity ‘epidemic’ we must tackle the parallel epidemic of weight stigma.
The most effective and ethical approaches will aim to address the behaviors and attitudes of the individuals and institutions that do the stigmatizing, rather than those of the targets of mistreatment [ 53 ], thus avoiding blaming the victim and removing the burden of change from those experiencing mistreatment. Such a pervasive problem requires a multi-pronged strategy both within healthcare settings and at higher levels of government and society. In healthcare settings, medical training must address weight bias. Healthcare professionals and students need to be educated about what weight bias is, how it is perpetuated, the subtle ways it manifests, and the effect that it has on their patients. Part of this training could include education regarding the research documenting the complex relationship between higher BMI and health [ 54 ], the well-documented shortcomings of BMI as an indicator of health [ 55 , 56 ], and important non-behavioral contributors to BMI such as genes [ 57 ] and diseases that create obesity as a symptom (e.g., polycystic ovary syndrome, lipedema, or hypothyroidism). Compassionate and knowledgeable healthcare providers will deliver better care, lessening the negative effects of weight bias. However, healthcare providers could go beyond merely not having bias to creating weight-inclusive [ 58 ], welcoming atmospheres. Such an approach focuses on well-being rather than weight loss and emphasizes healthy behaviors [ 13 , 58 ]. Empathy, respect, and humanity will foster better healthcare.
At a broader level, public health approaches to promoting metabolic health must stop the blame and shame implicit (and sometimes very explicit [ 59 ]) in their messaging. Public health messages speak not just to the target of the message but also to society more generally. Fat-shaming messages encourage discrimination by condoning it. Public health messages can encourage healthy behaviors without once mentioning weight or size by emphasizing that modifiable behaviors, such as an increase in fruit and vegetable intake and physical activity, better sleep patterns, and stress reduction, would improve health for all [ 13 , 60 , 61 ], regardless of the number on the scale.
Furthermore, there must be legal protection against weight-based discrimination. In the United States, for example, the Civil Rights Act of 1964 does not identify weight as a protected characteristic, and only in rare instances can people with very high BMI seek legal protection under Americans with Disabilities Act legislation. Drawing parallels from analyses of sexual orientation discrimination laws [ 26 ], we know that policies protecting higher-weight individuals will reduce the likelihood that prejudicial beliefs against stigmatized people are translated into damaging discriminatory treatment.
Influential people who fat shame, whether they are healthcare providers, parents, educators, business leaders, celebrities, or politicians, are the most damaging. They must be made aware of and held responsible for their behavior. Social attitudes likely change fastest when those with the most power serve as proper role models for a civil society or face negative consequences of their demeaning behavior [ 62 , 63 ]. However, who will call out those that are enacting prejudice? Healthcare providers may be ideal candidates to do so. Higher status individuals incur fewer social costs than lower status individuals when they recognize and claim discrimination happening to others [ 64 ]. Healthcare providers are conferred higher social status due to the imprimatur of medicine, and can thus serve as valuable allies for heavier individuals facing fat shaming.
Finally, public service messages are needed to educate people about the stigma, discrimination, and challenges facing higher-weight individuals; blatant discrimination must be stopped, but so too must the implicit [ 33 ] and daily [ 65 , 66 ] cultural biases against them. Weight stigma often happens in quiet and subtle ways that may be invisible to those doing the stigmatizing, yet hurtful and demoralizing to those on the receiving end. For example, a thinner patient may receive eye contact and a smile from a physician who walks into the room, whereas that same physician might avoid eye contact with a heavier patient; the daily nature of this form of weight stigma likely accumulates, ultimately harming health [ 67 ].
We have argued in this Opinion article that weight stigma poses a threat to health. There is a clear need to combat weight stigma, which is widespread worldwide [ 3 ] and, as we reviewed above, throughout healthcare settings. Doing so will help to improve the health and quality of life of millions of people. Indeed, eradicating weight stigma will likely improve the health of all individuals, regardless of their size, since the insidious effects of weight stigma reviewed herein are found independently of objective BMI, with many individuals with ‘normal’ BMI also falling prey to the health-harming processes brought about by weight stigmatization.
Enlightened societies should not treat its members with prejudice and discrimination because of how they look. Healthcare providers should treat obesity if patients have actual markers of poor metabolic health rather than simply due to their high BMI. Additionally, if patients request counseling regarding their metabolic health, healthcare providers can address actual behaviors, such as healthy eating and physical activity, without ever mentioning, and certainly without ever stigmatizing, a patient’s objective BMI [ 13 ]. Indeed, this is the strategy of interventions such as Health at Every Size ® [ 68 ] and other non-dieting approaches (reviewed in [ 69 ]), which have been shown in randomized controlled trials to improve multiple health outcomes such as blood pressure and cholesterol. The provider–patient relationship is one that is inherently unequal, with healthcare providers holding the power to profoundly affect patient’s thoughts, feelings, and behaviors [ 70 ]. To advance as an equal society, healthcare providers should lead the way for weight stigma eradication.
Abbreviations
Body mass index
Midlife in the United States
Richardson SA, Goodman N, Hastorf AH, Dornbusch SM. Cultural uniformity in reaction to physical disabilities. Am Sociol Rev. 1961;26(2):241–7.
Article Google Scholar
Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995-1996 through 2004-2006. Obesity. 2008;16(5):1129–34.
Article PubMed Google Scholar
Brewis AA, Wutich A, Falletta-Cowden A, Rodriguez-Soto I. Body norms and fat stigma in global perspective. Curr Anthropol. 2011;52(2):269–76.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17(5):941–64.
Puhl RM, Suh Y. Health consequences of weight stigma: implications for obesity prevention and treatment. Curr Obes Rep. 2015;4(2):182–90.
Spahlholz J, Baer N, König H-H, Riedel-Heller SG, Luck-Sikorski C. Obesity and discrimination - a systematic review and meta-analysis of observational studies. Obes Rev. 2016;17(1):43–55.
Article PubMed CAS Google Scholar
Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes. 2008;32(6):992–1000.
Article CAS Google Scholar
Fikkan JL, Rothblum ED. Is fat a feminist issue? Exploring the gendered nature of weight bias. Sex Roles. 2012;66(9):575–92.
Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity. 2014;22(4):1201–8.
Callahan D. Obesity: chasing an elusive epidemic. Hast Cent Rep. 2013;43(1):34–40.
Callahan D. Children, stigma, and obesity. JAMA Pediatr. 2013;167(9):791–2.
Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–28.
Article PubMed PubMed Central Google Scholar
Logel C, Stinson DA, Brochu PM. Weight loss is not the answer: a well-being solution to the “obesity problem”. Soc Personal Psychol Compass. 2015;9(12):678–95.
Major B, Tomiyama AJ, Hunger JM. The negative and bidirectional effects of weight stigma on health. In: Major B, Dovidio JF, Link BG, editors. The Oxford Handbook of Stigma, Discrimination, and Health; 2018. p. 499–519.
Google Scholar
Major B, Hunger JM, Bunyan DP, Miller CT. The ironic effects of weight stigma. J Exp Soc Psychol. 2014;51:74–80.
Schvey NA, Puhl RM, Brownell KD. The impact of weight stigma on caloric consumption. Obesity. 2011;19(10):1957–62.
Vartanian LR, Shaprow JG. Effects of weight stigma on exercise motivation and behavior: a preliminary investigation among college-aged females. J Health Psychol. 2008;13(1):131–8.
Hunger JM, Tomiyama AJ. Weight labeling and obesity. JAMA Pediatr. 2014;168(6):579–80.
Jackson SE, Beeken RJ, Wardle J. Perceived weight discrimination and changes in weight, waist circumference, and weight status. Obesity. 2014;22:2485–8.
Sutin AR, Terracciano A. Perceived weight discrimination and obesity. PLoS One. 2013;8(7):e70048.
Article PubMed PubMed Central CAS Google Scholar
Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. Psychol Sci. 2015;26(11):1803–11.
Sutin AR, Stephan Y, Luchetti M, Terracciano A. Perceived weight discrimination and C-reactive protein. Obesity. 2014;22(9):1959–61.
Tsenkova V, Carr D, Schoeller D, Ryff C. Perceived weight discrimination amplifies the link between central adiposity and nondiabetic glycemic control (HbA1c). Ann Behav Med. 2011;41(2):243–51.
Pearl RL, Wadden TA, Hopkins CM, et al. Association between weight bias internalization and metabolic syndrome among treatment-seeking individuals with obesity. Obesity. 2017;25(2):317–22.
Schafer MH, Ferraro KF. The stigma of obesity. Soc Psychol Q. 2011;74(1):76–97.
Hatzenbuehler ML, Keyes KM, Hasin DS. Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity. 2009;17(11):2033–9.
Hackman J, Maupin J, Brewis AA. Weight-related stigma is a significant psychosocial stressor in developing countries: evidence from Guatemala. Soc Sci Med. 2016;161:55–60.
Daly M, Robinson E, Sutin AR. Does knowing hurt? Perceiving oneself as overweight predicts future physical health and well-being. Psychol Sci. 2017;28(7):872–81.
Robinson E, Sutin AR. Parental perception of weight status and weight gain across childhood. Pediatrics. 2016;137(5):e20153957.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–26.
Puhl RM, Phelan SM, Nadglowski J, Kyle TK. Overcoming weight bias in the management of patients with diabetes and obesity. Clin Diabetes. 2016;34(1):44–50.
Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS One. 2012;7(11):e48448.
Tomiyama AJ, Finch LE, Belsky ACI, et al. Weight bias in 2001 versus 2013: contradictory attitudes among obesity researchers and health professionals. Obesity. 2015;23(1):46–53.
Adarns CH, Smith NJ, Wilbur DC, Grady KE. The relationship of obesity to the frequency of pelvic examinations: do physician and patient attitudes make a difference? Women Health. 1993;20(2):45–57.
Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for white and African-American obese women. Int J Obes. 2006;30(1):147–55.
Hebl MR, Xu J, Mason MF. Weighing the care: patients’ perceptions of physician care as a function of gender and weight. Int J Obes. 2003;27(2):269–75.
Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13(9):1615–23.
Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. 2005;46(3):244–59.
Puhl RM, Peterson JL, Luedicke J. Parental perceptions of weight terminology that providers use with youth. Pediatrics. 2011;128(4):e786–93.
Puhl RM, Peterson JL, Luedicke J. Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. Int J Obes. 2013;37(4):612–9.
Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Perceived judgment about weight can negatively influence weight loss: a cross-sectional study of overweight and obese patients. Prev Med (Baltim). 2014;62:103–7.
Phelan SM, Burgess DJ, Puhl RM, et al. The adverse effect of weight stigma on the well-being of medical students with overweight or obesity: findings from a national survey. J Gen Intern Med. 2015;30(9):1251–8.
Puhl RM, Moss-Racusin CA, Schwartz MB, Brownell KD. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res. 2008;23(2):347–58.
Fredrickson BL, Roberts TA, Noll SM, Quinn DM, Twenge JM. That swimsuit becomes you: sex differences in self-objectification, restrained eating, and math performance. J Pers Soc Psychol. 1998;75(1):269–84.
Dusenbery M. Doctors told her she was just fat. She actually had cancer. Cosmopolitan. 2018. https://www.cosmopolitan.com/health-fitness/a19608429/medical-fatshaming/ . Accessed 26 June 2018.
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387(10026):1377–96.
Abarca-Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42.
GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Krueger PM, Reither EN. Mind the gap: race/ethnic and socioeconomic disparities in obesity. Curr Diab Rep. 2015;15(11):95.
Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci. 2014;111(4):1338–42.
Mensink GBM, Schienkiewitz A, Haftenberger M, Lampert T, Ziese T, Scheidt-Nave C. Übergewicht und Adipositas in Deutschland. Bundesgesundheitsblatt - Gesundheitsforsch - Gesundheitsschutz. 2013;56(5–6):786–94.
Moore JX, Chaudhary N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and nutrition examination survey, 1988–2012. Prev Chronic Dis. 2017;14:160287.
Pearl RL. Weight bias and stigma: public health implications and structural solutions. Soc Issues Policy Rev. 2018;12(1):146–82.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82.
Tomiyama AJ, Hunger JM, Nguyen-Cuu J, Wells C. Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005-2012. Int J Obes. 2016;40(5):883–6.
Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes. 2008;32:S56–9.
Bell CG, Walley AJ, Froguel P. The genetics of human obesity. Nat Rev Genet. 2005;6(3):221–34.
Tylka TL, Annunziato RA, Burgard D, et al. The weight-inclusive versus weight-normative approach to health: evaluating the evidence for prioritizing well-being over weight loss. J Obes. 2014;2014:983495.
Teegardin C. Grim childhood obesity ads stir critics. The Atlanta Journal Constitution. 2012. https://www.ajc.com/news/local/grim-childhood-obesity-ads-stir-critics/GVsivE43BYQAqe6bmufd7O/ . Accessed 26 June 2018.
Chiang JJ, Turiano NA, Mroczek DK, Miller GE. Affective reactivity to daily stress and 20-year mortality risk in adults with chronic illness: findings from the National Study of daily experiences. Health Psychol. 2018;37(2):170–8.
Carroll JE, Seeman TE, Olmstead R, et al. Improved sleep quality in older adults with insomnia reduces biomarkers of disease risk: pilot results from a randomized controlled comparative efficacy trial. Psychoneuroendocrinology. 2015;55:184–92.
Dasgupta N, Greenwald AG. On the malleability of automatic attitudes: combating automatic prejudice with images of admired and disliked individuals. J Pers Soc Psychol. 2001;81(5):800–14.
French JRP, Raven B. The bases of social power. In: Cartwright D, editor. Studies in social power. Ann Arbor: Institute for Social Research, University of Michigan; 1959. p. 150–67.
Eliezer D, Major B. It’s not your fault: the social costs of claiming discrimination on behalf of someone else. Gr Process Intergr Relat. 2012;15(4):487–502.
Seacat JD, Dougal SC, Roy D. A daily diary assessment of female weight stigmatization. J Health Psychol. 2016;21(2):228–40.
Vartanian LR, Pinkus RT, Smyth JM. The phenomenology of weight stigma in everyday life. J Context Behav Sci. 2014;3(3):196–202.
Vartanian LR, Pinkus RT, Smyth JM. Experiences of weight stigma in everyday life: implications for health motivation. Stigma Heal. 2018;3(2):85–92.
Bacon L. Health at every size: the surprising truth about your weight. Dallas: BenBella Books Inc.; 2008.
Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr J. 2011;10(1):9.
Hall JA, Roter DL. Physician–patient communication. In: Friedman HS, editor. The Oxford handbook of Health Psychology. Oxford: Oxford University Press; 2011.
Download references
Acknowledgements
We thank the Virginia G. Piper Charitable Trust and Mayo Clinic-ASU Obesity Solutions for supporting the workshop that that allowed us to work together on this piece.

Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and affiliations.
Department of Psychology, University of California Los Angeles, 1285 Franz Hall, Los Angeles, CA, 90095, USA
A. Janet Tomiyama
Department of Sociology, Boston University, Boston, MA, USA
Deborah Carr
Department of Sociology, Anthropology, and Criminal Justice, Clemson University, Clemson, SC, USA
Ellen M. Granberg
Department of Psychological and Brain Sciences, University of California, Santa Barbara, CA, USA
Brenda Major
Institute of Psychology, Health and Society, University of Liverpool, Liverpool, UK
Eric Robinson
Department of Behavioral Sciences and Social Medicine, Florida State University College of Medicine, Tallahassee, FL, USA
Angelina R. Sutin
School of Human Evolution and Social Change, Arizona State University, Tempe, AZ, USA
Alexandra Brewis
You can also search for this author in PubMed Google Scholar
Contributions
AJT wrote the first draft of the manuscript. All authors read and approved the final manuscript. Authors are listed alphabetically aside from the first and last authors.
Corresponding author
Correspondence to A. Janet Tomiyama .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Tomiyama, A., Carr, D., Granberg, E. et al. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Med 16 , 123 (2018). https://doi.org/10.1186/s12916-018-1116-5
Download citation
Received : 12 March 2018
Accepted : 03 July 2018
Published : 15 August 2018
DOI : https://doi.org/10.1186/s12916-018-1116-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Weight stigma
- Weight bias
- Anti-fat attitudes
- Discrimination
- Health policy
BMC Medicine
ISSN: 1741-7015
- General enquiries: [email protected]
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Impact of weight bias and stigma on quality of care and outcomes for patients with obesity
Wl hellerstedt.
- Author information
- Article notes
- Copyright and License information
Address for correspondence: Dr SM Phelan, Division of Health Care Policy and Research, Mayo Clinic, 200 First St SW, Rochester, MN 55905, USA., E-mail: [email protected]
Received 2014 Oct 25; Revised 2014 Dec 19; Accepted 2015 Jan 7; Issue date 2015 Apr.
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs License, which permits use and distribution in any medium, provided the original work is properly cited, the use is non-commercial and no modifications or adaptations are made.
The objective of this study was to critically review the empirical evidence from all relevant disciplines regarding obesity stigma in order to (i) determine the implications of obesity stigma for healthcare providers and their patients with obesity and (ii) identify strategies to improve care for patients with obesity. We conducted a search of Medline and PsychInfo for all peer-reviewed papers presenting original empirical data relevant to stigma, bias, discrimination, prejudice and medical care. We then performed a narrative review of the existing empirical evidence regarding the impact of obesity stigma and weight bias for healthcare quality and outcomes. Many healthcare providers hold strong negative attitudes and stereotypes about people with obesity. There is considerable evidence that such attitudes influence person-perceptions, judgment, interpersonal behaviour and decision-making. These attitudes may impact the care they provide. Experiences of or expectations for poor treatment may cause stress and avoidance of care, mistrust of doctors and poor adherence among patients with obesity. Stigma can reduce the quality of care for patients with obesity despite the best intentions of healthcare providers to provide high-quality care. There are several potential intervention strategies that may reduce the impact of obesity stigma on quality of care.
Keywords: Delivery of health care, obesity, stereotyping, social stigma
Introduction
The goal of primary care is to improve patients' health, longevity and quality of life through the provision of patient-centred care. To do so, healthcare providers must identify modifiable behaviours that increase disease risk, and help patients change them. Recent US Preventive Services Task Force guidelines recommend screening adults for obesity and offering behavioural interventions to those with a body mass index (BMI) over 30 kg m −2 ( 1 ). However, obesity is a stigmatized condition; thus, one side effect of increased focus on body weight in health care may be the alienation and humiliation of these patients. The term ‘stigma’ describes physical characteristics or character traits that mark the bearer as having lower social value ( 2 ). A stigmatized trait can lead to experiences of discrimination, and the feeling of being stigmatized can put one at risk for low self-esteem ( 3 ), depression ( 4 – 6 ) and lower quality of life ( 7 – 10 ). However, the empirical evidence on stigma overall and obesity stigma in particular is scattered across diverse disciplines and lines of research, making it difficult to get a clear picture of the implication of obesity stigma for healthcare providers and their patients.
In order to address this gap, we critically reviewed literature related to the impact of obesity stigma on interpersonal encounters and decision-making. We discuss potential implications, including several mechanisms whereby stigma may affect patient-centred communication and care, defined by the Institute of Medicine ( 11 ) as ‘care that establishes a partnership among practitioners, patients, and their families (when appropriate) to ensure that decisions respect patients' wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care’ (p. 7). We also suggest several strategies that may help healthcare providers and clinics reduce the impact of stigma on patients with obesity.
Obesity is a commonly and strongly stigmatized characteristic ( 12 , 13 ). There is substantial empirical evidence that people with obesity elicit negative feelings such as disgust, anger, blame and dislike in others ( 14 – 16 ). Despite the high prevalence of obesity (approximately one-third of the US adult population ( 17 ) ), individuals with obesity are frequently the targets of prejudice, derogatory comments and other poor treatment in a variety of settings, including health care ( 12 , 18 ). Furthermore, there is a growing body of evidence that physicians and other healthcare professionals hold strong negative opinions about people with obesity ( 19 – 27 ).
We conducted a narrative review of this literature to highlight the ways that the obesity stigma may interrupt the healthcare process and impede many healthcare providers' goal of providing equitable high-quality care. We reviewed all original studies in the fall of 2014 on topics related to obesity stigma in medical care and/or the impact of stigma on interpersonal encounters and decision-making in PubMed and PsychInfo, with the majority of studies found in health communication, social psychology and health disparities research. We then selected papers relevant to the potential impact of obesity stigma on healthcare provider behaviour, patient healthcare outcomes and healthcare encounters.
Impact on providers
Primary care providers and health promotion specialists, who typically demonstrate a commitment to providing care for underserved populations, are unlikely to flagrantly and intentionally discriminate against their patients. Nevertheless, there are several ways that their attitudes about obesity may cause their patients with obesity to feel disrespected, inadequate or unwelcome, thus negatively affecting the encounter quality and their willingness to seek needed care (see Fig. 1 ). Behaviours that emanate from negative attitudes about a stigmatized group are known as enacted stigma ( 28 ). Enacted stigma on the part of the provider affects the patient in both measurable and immeasurable ways. It can reduce the quality, and even the quantity, of patient-centred care, and can signal to the patient that he or she is being perceived in terms of his or her stigmatized identity, which, in turn, may affect patient perception of, and compliance with, provider recommendations.
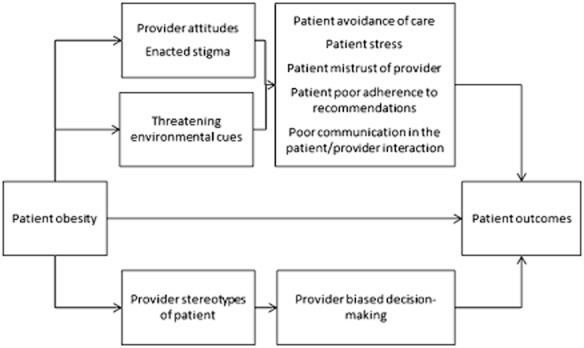
A conceptual model of hypothesized pathways whereby the associations between obesity and health outcomes are partially mediated by healthcare providers' attitudes and behaviours about obese patients, and patients' response to feeling stigmatized.
The negative attitudes underlying enacted stigma can be explicit or implicit. Explicit attitudes are conscious and reflect a person's opinions or beliefs about a group. Implicit attitudes are automatic and often occur outside of awareness and in contrast to explicitly held beliefs ( 29 ). The response to some stigmatized groups, such as racial minorities among egalitarian Caucasians, often consists of negative implicit attitudes, but neutral or positive explicit ones ( 30 ). In contrast, explicit negative attitudes about people with obesity are more socially acceptable than explicit racism: e.g. it is acceptable in many Western cultures that people with obesity are the source of derogatory humour and may thus be openly – and unquestionably – portrayed as lazy, gluttonous and undisciplined. Primary care providers, medical trainees, nurses and other healthcare professionals hold explicit as well as implicit negative opinions about people with obesity ( 21 , 31 – 33 ). This has important implications for communication in the clinical interview, because explicit attitudes influence verbal behaviours as well as decisions that are within conscious control, whereas implicit negative attitudes predict non-verbal communication and decisions under cognitive burden ( 29 , 34 – 36 ). There is evidence that providers' communication is less patient-centred with members of stigmatized racial groups ( 37 – 43 ), and other stigmatized groups including patients with obesity ( 44 ), and that provider attitudes contribute to this disparity ( 45 – 47 ). Implicit attitudes have also been found to be associated with lower patient ratings of care ( 46 ). The combination of implicit and explicit negative obesity attitudes may elevate the potential for impaired patient-centred communication, which is associated with a 19% higher risk of patient non-adherence, as well as mistrust, and worse patient weight loss, recovery and mental health outcomes ( 48 – 53 ).
There are several mechanisms by which provider attitudes may affect the quality of, or potential for, patient-centred care. First, primary care providers engage in less patient-centred communication with patients they believe are not likely to be adherent ( 54 ). A common explicitly endorsed provider stereotype about patients with obesity is that they are less likely to be adherent to treatment or self-care recommendations ( 23 , 24 , 55 , 56 ), are lazy, undisciplined and weak-willed ( 12 , 55 , 57 – 59 ). Second, primary care providers have reported less respect for patients with obesity compared with those without ( 59 , 60 ), and low respect has been shown to predict less positive affective communication and information giving ( 61 ). Third, primary healthcare providers may allocate time differently, spending less time educating patients with obesity about their health ( 62 ). For example, in one study of primary care providers randomly assigned to evaluate the records of patients who were either obese or normal weight, providers who evaluated patients who were obese were more likely to rate the encounter as a waste of time and indicated that they would spend 28% less time with the patient compared with those who evaluated normal-weight patients ( 59 ). Finally, physicians may over-attribute symptoms and problems to obesity, and fail to refer the patient for diagnostic testing or to consider treatment options beyond advising the patient to lose weight. In one study involving medical students, virtual patients with shortness of breath were more likely to receive lifestyle change recommendations if they were obese (54% vs. 13%), and more likely to receive medication to manage symptoms if they were normal weight (23% vs. 5%) ( 23 ).
Impact on patients
Experiences of discrimination and awareness of stigmatized social status can cause patients to experience stress and have other acute reactions that may reduce the quality of the encounter, regardless of their provider's attitudes and behaviour. Three conceptually overlapping processes – identity threat, stereotype threat and felt stigma – describe the stigmatized patient's reaction to being stigmatized. Identity threat occurs when patients experience situations that make them feel devalued because of a social identity. Social identities are the categories, roles, and social groups that define each person and give a sense of self ( 63 , 64 ). Each social identity, be it a professional identity, a gender identity, or identity as a person who is obese, has emotional significance for the individual, is closely tied to self-esteem, and can empower or make one vulnerable. Obesity is stigmatized, and thus is more likely to make the individual aware of the possibility for rejection or derogation than make him/her feel confident and empowered. Stereotype threat occurs when an individual is aware that he or she may be viewed as a member of a stigmatized group, and becomes preoccupied with detecting stereotyping on the part of the provider and monitoring his or her own behaviour to ensure that it does not confirm group stereotypes ( 65 ). Felt stigma is a term used to describe the expectation of poor treatment based on past experiences of discrimination ( 28 ).
The effects of stigma are both immediate and long-term. The direct effects of provider attitudes on patient-centred care may reduce the quality of the patient encounter, harming patient outcomes and reducing patient satisfaction. Patients with obesity who experience identity/stereotype threat or felt/enacted stigma may experience a high level of stress which can contribute to impaired cognitive function and ability to effectively communicate ( 66 ). Accumulated exposure to high levels of stress hormones (allostatic load) has several long-term physiological health effects, including heart disease, stroke, depression and anxiety disorder, diseases that disproportionately affect obese individuals and have been empirically linked to perceived discrimination ( 67 – 69 ). Indeed, stress pathways may present an alternate explanation for some proportion of the association between obesity and chronic disease ( 70 ).
Other effects include avoidance of clinical care if patients perceive that their body weight will be a source of embarrassment in that setting ( 71 , 72 ). For example, there is evidence that obese women are less likely to seek recommended screening for some cancers ( 72 – 76 ). The long-term result of avoidance and postponement of care is that people with obesity may present with more advanced, and thus more difficult to treat, conditions. Individuals who are stigmatized, or are vigilant for evidence of stigma, may withdraw from full participation in the encounter. Because of this, they may not recall advice or instructions given by the provider, reducing adherence to prescribed treatment or self-care. Experiencing stereotype threat may also cause patients to discount feedback provided by the source of the threat ( 77 ), which in turn may affect adherence. Patients who report feeling judged by their primary care provider are less likely to seek or achieve successful weight loss ( 78 , 79 ). Patients who have tried to lose weight and failed may ‘dis-identify’, or reduce their efforts to lose weight, in order to disconnect their self-esteem from achievement in a domain with which they have not had success ( 65 ), and may feel shame for failing to lose weight or maintain weight loss ( 78 ). Along similar lines, individuals who experience more obesity stigma report less health utility, or place lower value on health ( 80 ).
Setting factors
Felt stigma and identity/stereotype threat can be triggered by experiences in the healthcare clinical setting that signal to the patient that his/her identity as a person who is obese is salient and possibly devalued. A typical primary care clinical encounter has many such signals, including weight measurement, dietary assessment, and queries about physical activity. Providers are also encouraged to provide unsolicited weight loss counsel as well as to assess patients' willingness to alter behaviours that are associated with obesity. There is evidence that many providers dislike treating obesity, feel underprepared to do so, and have little hope that their patients will make lifestyle changes ( 55 , 81 – 84 ), which may be detectable in their tone of voice or language. They may also signal overly simplified assumptions about the causes of obesity, by suggesting, for example, that their patients cut back on fast food or consider taking the stairs instead of elevators. These assumptions ignore the complexity of energy balance and propagate a common misunderstanding that weight loss is as simple as ‘calories in < calories out’ ( 85 ). Such counsel, despite its positive intentions to optimize patient health, may create unrealistic expectations about the effects of small lifestyle changes, which may lead to disappointment and recidivism. This counsel can also have unintended side effects if it signals to patients that they are seen solely in terms of their stigmatized identity. This could create a state of threat that may affect the patient's emotional state, ability to communicate effectively, and attitude towards medical advice ( 86 ).
Clinic equipment may also promote identity threat for patients with obesity ( 87 , 88 ). Waiting room chairs with armrests can be uncomfortable or too small. Equipment such as scales, blood pressure cuffs, examination gowns and pelvic examination instruments are often designed for use with smaller patients. When larger alternatives are not available, or are stored in a place that suggests infrequent use, it can signal to patients that their size is unusual and that they do not belong. These experiences, which are not delivered with malicious intent, can be humiliating.
Potential strategies to address obesity stigma in clinical care
Promising strategies to reduce stigma in the primary care setting include improving provider attitudes about patients with obesity and/or reducing the likelihood that negative attitudes influence provider behaviour; altering the clinic environment or procedures to create a setting where patients with obesity feel accepted and less threatened; and empowering patients to cope with stigmatizing situations and attain high-quality health care ( 86 , 89 ). Here we focus on strategies that clinics or healthcare organizations might implement to improve the experience of patients with obesity or overweight. Some of the studies discussed here are firmly rooted in research evidence, but some are untested strategies that will require research to test their effectiveness.
Our intent was to highlight the salience of obesity stigma in health care and the potential to re-frame and optimize provider–patient encounters. Our work recognizes the contributions of interdisciplinary scholars, in fat studies and elsewhere, who have raised awareness of how cultures conceptualize body size, and consequently, how body size itself can inform identity. Such scholars have thus set much of the theoretical foundation for our work, even though our suggestions are not consistent with their advocacy for a weight-inclusive approach to medical care, in which obesity is seen as independent of health and weight reduction is not a focus of medical care ( 90 , 91 ). While there is evidence supporting this viewpoint, we focus on interventions that are more consistent with the dominant medical and nursing paradigms of obesity as a risk factor.
Reducing weight stigma in clinical care is a shared responsibility of healthcare providers and other clinic staff, as well as the healthcare systems/organizations that have the power to implement intervention strategies broadly. Many of the strategies we discuss here can be implemented by providers or clinics, but any of these strategies could be implemented more efficiently, and have a wider influence, if uptake was required of providers and clinic staff by healthcare organizations.
Strategies that clinics can implement to improve provider attitudes about people with obesity include the following. (i) Increase provider empathy through perspective-taking exercises. Perspective-taking exercises have improved provider attitudes towards stigmatized groups ( 92 ), although findings are mixed about its effectiveness in reducing obesity stigma ( 93 , 94 ). (ii) Alter perceived norms regarding negative attitudes and stereotypes about people with obesity. In one study, researchers reduced explicit bias against obese people by providing individuals information and evidence that their peers did not hold negative attitudes ( 95 ). To minimize the perception that anti-fat bias is the norm, one untested strategy could include implementing a zero-tolerance policy for comments or humour that stereotypes or degrades anyone based on a physical identity or attribute. (iii) Encourage provider instruction and practice in emotion regulation techniques that foster positive affect. High cognitive load and time pressure, characteristic of clinical care settings, impair judgments and decision-making ( 96 ). Furthermore, frustration that providers may feel towards ‘difficult’ or ‘complex’ patients or patients who they perceive are harming their own health, may elicit strong negative emotions. Although no studies have directly tested their effect on weight bias, evidence from one study of prejudice reduction suggests that emotion regulation tools such as meditation or deep breathing may help providers overcome these negative emotions and improve compassion and other pro-social emotions ( 97 , 98 ). (iv) An untested strategy to build awareness of weight bias and a felt need to address it might include encouraging providers to examine their explicit beliefs and stereotypes about obese people, and complete an assessment of implicit attitudes (e.g. the online Implicit Association Test at http://www.implicit.harvard.edu ). Provide information about the automatic nature of these attitudes and encourage providers to consciously strive to behave in ways consistent with helping and egalitarian values. And lastly, (v) educate providers on the genetic, environmental, biological, psychological and social contributors to weight gain and loss ( 99 , 100 ). Providers who understand this complex web of causality have more positive attitudes about patients with obesity ( 101 ). This information is likely less threatening for their patients than over-simplified messages like ‘eat less, move more’, or ‘calories in, calories out’ ( 102 ).
There are several strategies for providing a welcoming and less threatening healthcare environment to patients with obesity. (i) Reduce focus on body weight. Instead, focus on screening for the diseases and conditions for which obesity is a risk factor and encourage feasible behaviours that will improve health and well-being. This could be accomplished by weighing patients less frequently – for example, restricting weigh-ins to well-visit checkups and forgoing weigh-ins when visits are not associated with a weight-related reason. Increasing patients' knowledge of the health effects of obesity has shown little effect on weight loss ( 103 , 104 ). However, encouraging patients to not focus on weight or weight loss, but rather on the other benefits of physical activity and healthy eating, may reduce the threat of conversations about these behaviours, and thus increase the likelihood of behaviour change and maintenance ( 102 , 105 ). (ii) Adopt patient-centred communication strategies, such as motivational interviewing, which may be less threatening for patients and are associated with patient adherence and positive outcomes ( 48 , 51 – 53 , 106 – 108 ). (iii) Although its impact on felt stigma is not tested, one could ensure that the clinic environment is welcoming by providing chairs and medical equipment that are usable by patients of all sizes and by keeping specialized instruments for patients with obesity readily available to clinical staff. (iv) Convey a sense of identity safety by providing evidence that diversity is valued ( 109 ). Although untested, this could be accomplished by posting a mission statement that stresses the value of body size diversity or by using positive and non-stereotypical images of overweight and obese people in clinic advertisements, pamphlets or artwork. (v) Healthcare systems could ensure that the continuum of care includes adequate referral resources for behaviour change counselling, including providers or clinics specializing in weight loss strategies and remove barriers (e.g. requirement for a secondary diagnosis, long wait times for an appointment) to accessing these resources ( 78 ). Study is needed in this area to determine whether shifting the threat of discussing weight loss strategies from the primary care setting to a specialty care setting may improve utilization of primary health care. These providers may also be more skilled at using communication strategies that are not threatening.
Healthcare providers strive to provide the highest quality health care for their patients. This effort may be hindered by interpersonal and environmental cues that convey that patients with obesity are not welcome or by behaviours that lower the quality of communication in the encounter. Attitudes towards obesity as a health risk factor can exacerbate and mask negative attitudes towards individuals with obesity. Healthcare providers often view obesity as an avoidable risk factor that impedes their ability to treat and prevent disease. As this is a largely unchallenged perspective on obesity , healthcare providers may be less self-aware of their propensity to, and feel less pressure (internally or from external sources) to, behave in a non-prejudicial way towards people with obesity .
A great deal more research is needed to understand the impact of stigma on care for people with obesity. Much of the extant research involves small or convenience samples and requires replication with more generalizable populations. There are several important gaps in the literature on weight bias and health care. While several studies have found high levels of explicit bias in healthcare providers, there is a need for more research on weight stigma using measures of implicit bias. More research is also needed to identify the impact of those attitudes on aspects of the medical encounter, including decision-making and communication, as well as the differential effects of those attitudes by gender, race, socioeconomic status, sexual orientation, and other characteristics. The development and testing of novel interventions is also needed to reduce bias or its impact on behaviour in medical trainees, practicing physicians, other healthcare providers, and other staff members of healthcare organizations.
It is important to note the tension between obesity stigma literature or literature advocating a weight-inclusive approach ( 91 ) and the body of literature that supports increased provider attention to body weight and weight loss as a strategy to encourage behaviour change. We believe that the strategies and perspectives reviewed here are not contrary to this evidence, but may inform the refinement of interventions in order to avoid unintended consequences brought on by stigma, and maximize the effectiveness of patient behaviour change intervention.
Acknowledgments
Dr. Phelan is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K01DK095924. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement
Drs. Burgess, Hellerstedt, Griffin, and van Ryn do not report any potential conflicts of interest. Dr. Phelan and Dr. Yeazel report grants from the National Institutes of Health during the conduct of the study.
- 1. Moyer VA, on behalf of the United States Preventive Services Task Force Screening for and management of obesity in Adults: U.S. preventive services task force recommendation statement. Ann Intern Med. 2012;157:1–32. doi: 10.7326/0003-4819-157-5-201209040-00475. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs: Prentice-Hall; 1963. [ Google Scholar ]
- 3. Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: the consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Serv. 2001;52:1621–1626. doi: 10.1176/appi.ps.52.12.1621. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Phelan SM, Griffin JM, Jackson GL, et al. Stigma, perceived blame, self-blame, and depressive symptoms in men with colorectal cancer. Psychooncology. 2013;22:65–73. doi: 10.1002/pon.2048. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Phelan SM, Griffin JM, Hellerstedt WL, et al. Perceived stigma, strain, and mental health among caregivers of veterans with traumatic brain injury. Disabil Health J. 2011;4:177–184. doi: 10.1016/j.dhjo.2011.03.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21:1007–1013. doi: 10.1080/09540120802614358. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Markowitz FE. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav. 1998;39:335–347. [ PubMed ] [ Google Scholar ]
- 8. Major B, O'Brien LT. The social psychology of stigma. Annu Rev Psychol. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Myers A, Rosen JC. Obesity stigmatization and coping: relation to mental health symptoms, body image, and self-esteem. Int J Obes Relat Metab Disord. 1999;23:221–230. doi: 10.1038/sj.ijo.0800765. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Committee on the National Quality Report on Health Care Delivery. Envisioning the national health care quality report. In: Hurtado MP, Swift EK, Corrigan JM, editors. Board on Health Care Services. Washington, DC: National Academy Press; 2001. p. 256. [ PubMed ] [ Google Scholar ]
- 12. Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Latner JD, O'Brien KS, Durso LE, Brinkman LA, MacDonald T. Weighing obesity stigma: the relative strength of different forms of bias. Int J Obes (Lond) 2008;32:1145–1152. doi: 10.1038/ijo.2008.53. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Vartanian LR. Disgust and perceived control in attitudes toward obese people. Int J Obes (Lond) 2010;34:1302–1307. doi: 10.1038/ijo.2010.45. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Wear D, Aultman JM, Varley JD, Zarconi J. Making fun of patients: medical students' perceptions and use of derogatory and cynical humor in clinical settings. Acad Med. 2006;81:454–462. doi: 10.1097/01.ACM.0000222277.21200.a1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Puhl RM, Luedicke J, Grilo CM. Obesity bias in training: attitudes, beliefs, and observations among advanced trainees in professional health disciplines. Obesity (Silver Spring) 2014;22:1008–1015. doi: 10.1002/oby.20637. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Tomiyama AJ, Finch LE, Incollingo Belsky AC, et al. Weight bias in 2001 versus 2013: contradictory attitudes among obesity researchers and health professionals. Obesity (Silver Spring) 2014;23:46–53. doi: 10.1002/oby.20910. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring) 2013;22:1201–1208. doi: 10.1002/oby.20687. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Hebl MR, Xu J, Mason MF. Weighing the care: patients' perceptions of physician care as a function of gender and weight. Int J Obes Relat Metab Disord. 2003;27:269–275. doi: 10.1038/sj.ijo.802231. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Persky S, Eccleston CP. Medical student bias and care recommendations for an obese versus non-obese virtual patient. Int J Obes (Lond) 2010;35:728–735. doi: 10.1038/ijo.2010.173. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Puhl R, Wharton C, Heuer C. Weight bias among dietetics students: implications for treatment practices. J Am Diet Assoc. 2009;109:438–444. doi: 10.1016/j.jada.2008.11.034. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Wigton RS, McGaghie WC. The effect of obesity on medical students' approach to patients with abdominal pain. J Gen Intern Med. 2001;16:262–265. doi: 10.1046/j.1525-1497.2001.016004262.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Neumark-Sztainer D, Story M, Harris T. Beliefs and attitudes about obesity among teachers and school health care providers working with adolescents. J Nutr Educ. 1999;31:3–9. [ Google Scholar ]
- 27. Robertson N, Vohora R. Fitness vs. fatness: implicit bias toward obesity among fitness professionals and regular exercisers. Psychol Sport Exerc. 2008;9:547–557. [ Google Scholar ]
- 28. Jacoby A. Felt versus enacted stigma: a concept revisited. Evidence from a study of people with epilepsy in remission. Soc Sci Med. 1994;38:269–274. doi: 10.1016/0277-9536(94)90396-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Dovidio J, Kawakami K, Johnson C, Johnson B, Howard A. On the nature of prejudice: automatic and controlled processes. J Exp Soc Psychol. 1997;33:510–540. [ Google Scholar ]
- 30. Gaertner SL, Dovidio JF. The aversive form of racism. In: Dovidio JF, Gaertner SL, editors. Prejudice, Discrimination, and Racism. Orlando, FL: Academic Press; 1986. pp. 61–89. [ Google Scholar ]
- 31. Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Budd GM, Mariotti M, Graff D, Falkenstein K. Health care professionals' attitudes about obesity: an integrative review. Appl Nurs Res. 2009;24:127–137. doi: 10.1016/j.apnr.2009.05.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97:17–41. doi: 10.1037/a0015575. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Dovidio J, Kawakami K, Gaertner S. Implicit and explicit prejudice and interracial interaction. J Pers Soc Psychol. 2002;82:62–68. doi: 10.1037//0022-3514.82.1.62. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Gordon HS, Street RL, Jr, Sharf BF, Kelly PA, Souchek J. Racial differences in trust and lung cancer patients' perceptions of physician communication. J Clin Oncol. 2006;24:904–909. doi: 10.1200/JCO.2005.03.1955. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Gordon HS, Street RL, Jr, Sharf BF, Souchek J. Racial differences in doctors' information-giving and patients' participation. Cancer. 2006;107:1313–1320. doi: 10.1002/cncr.22122. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA. Patient-physician communication in the primary care visits of African Americans and whites with depression. J Gen Intern Med. 2008;23:600–606. doi: 10.1007/s11606-008-0539-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Cene CW, Roter D, Carson KA, Miller ER, III, Cooper LA. The effect of patient race and blood pressure control on patient–physician communication. J Gen Intern Med. 2009;24:1057–1064. doi: 10.1007/s11606-009-1051-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Beach MC, Saha S, Korthuis PT, et al. Differences in patient-provider communication for Hispanic compared to non-Hispanic white patients in HIV care. J Gen Intern Med. 2010;25:682–687. doi: 10.1007/s11606-010-1310-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Beach MC, Saha S, Korthuis PT, et al. Patient–provider communication differs for Black compared to White HIV-infected patients. AIDS Behav. 2010;15:805–811. doi: 10.1007/s10461-009-9664-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient–physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity (Silver Spring) 2013;21:2146–2152. doi: 10.1002/oby.20384. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Cooper L. Overcoming Healthcare Disparities: The Role of Patient-Centered Care. College of Public Health and Health Professions Celebrating 50 Years. Gainesville: University of Florida; 2008. [ Google Scholar ]
- 46. Penner LA, Dovidio JF, West TV, et al. Aversive racism and medical interactions with black patients: a field study. J Exp Soc Psychol. 2010;46:436–440. doi: 10.1016/j.jesp.2009.11.004. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Cooper L, Roter D, Carson K, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12:709–723. doi: 10.1111/j.1467-789X.2011.00892.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Jay M, Gillespie C, Schlair S, Sherman S, Kalet A. Physicians' use of the 5As in counseling obese patients: is the quality of counseling associated with patients' motivation and intention to lose weight? BMC Health Serv Res. 2010;10:159. doi: 10.1186/1472-6963-10-159. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 51. Fiscella K, Meldrum S, Franks P, et al. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42:1049–1055. doi: 10.1097/00005650-200411000-00003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Wanzer MB, Booth-Butterfield M, Gruber K. Perceptions of health care providers' communication: relationships between patient-centered communication and satisfaction. Health Commun. 2004;16:363–383. doi: 10.1207/S15327027HC1603_6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [ PubMed ] [ Google Scholar ]
- 54. Street RL, Jr, Gordon H, Haidet P. Physicians' communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65:586–598. doi: 10.1016/j.socscimed.2007.03.036. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. Foster GD, Wadden TA, Makris AP, et al. Primary care physicians' attitudes about obesity and its treatment. Obes Res. 2003;11:1168–1177. doi: 10.1038/oby.2003.161. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Huizinga MM, Bleich SN, Beach MC, Clark JM, Cooper LA. Disparity in physician perception of patients' adherence to medications by obesity status. Obesity (Silver Spring) 2010;18:1932–1937. doi: 10.1038/oby.2010.35. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 57. Harvey EL, Hill AJ. Health professionals' views of overweight people and smokers. Int J Obes Relat Metab Disord. 2001;25:1253–1261. doi: 10.1038/sj.ijo.0801647. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Puhl R, Brownell K. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Hebl MR, Xu J. Weighing the care: physicians' reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25:1246–1252. doi: 10.1038/sj.ijo.0801681. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach MC. Physician respect for patients with obesity. J Gen Intern Med. 2009;24:1236–1239. doi: 10.1007/s11606-009-1104-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians' attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ Couns. 2006;62:347–354. doi: 10.1016/j.pec.2006.06.004. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13:1615–1623. doi: 10.1038/oby.2005.198. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Tajfel H. Social psychology of intergroup relations. Annu Rev Psychol. 1982;33:1–39. [ Google Scholar ]
- 64. Hogg MA, Terry DJ. Social identity and self-categorization processes in organizational contexts. Acad Manage Rev. 2000;25:121–140. [ Google Scholar ]
- 65. Steele CM. A threat in the air. How stereotypes shape intellectual identity and performance. Am Psychol. 1997;52:613–629. doi: 10.1037//0003-066x.52.6.613. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Schmader T, Johns M, Forbes C. An integrated process model of stereotype threat effects on performance. Psychol Rev. 2008;115:336–356. doi: 10.1037/0033-295X.115.2.336. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 67. Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2008;98:S29–S37. doi: 10.2105/ajph.98.supplement_1.s29. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 69. Lewis TT, Everson-Rose SA, Powell LH, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African–American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [ DOI ] [ PubMed ] [ Google Scholar ]
- 70. Muennig P. The body politic: the relationship between stigma and obesity-associated disease. BMC Public Health. 2008;8:128. doi: 10.1186/1471-2458-8-128. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14:554–561. doi: 10.1111/j.1745-7599.2002.tb00089.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African–American obese women. Int J Obes (Lond) 2006;30:147–155. doi: 10.1038/sj.ijo.0803105. [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Cohen SS, Palmieri RT, Nyante SJ, et al. Obesity and screening for breast, cervical, and colorectal cancer in women: a review. Cancer. 2008;112:1892–1904. doi: 10.1002/cncr.23408. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Rosen AB, Schneider EC. Colorectal cancer screening disparities related to obesity and gender. J Gen Intern Med. 2004;19:332–338. doi: 10.1111/j.1525-1497.2004.30339.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 75. Aldrich T, Hackley B. The impact of obesity on gynecologic cancer screening: an integrative literature review. J Midwifery Womens Health. 2010;55:344–356. doi: 10.1016/j.jmwh.2009.10.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Fontaine KR, Faith MS, Allison DB, Cheskin LJ. Body weight and health care among women in the general population. Arch Fam Med. 1998;7:381–384. doi: 10.1001/archfami.7.4.381. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Cohen GL, Steele CM, Ross LD. The mentor's dilemma: providing critical feedback across the racial divide. Pers Soc Psychol Bull. 1999;25:1302–1318. [ Google Scholar ]
- 78. Thomas SL, Hyde J, Karunaratne A, Kausman R, Komesaroff PA. ‘They all work … when you stick to them’: a qualitative investigation of dieting, weight loss, and physical exercise, in obese individuals. Nutr J. 2008;7:34. doi: 10.1186/1475-2891-7-34. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Perceived judgment about weight can negatively influence weight loss: a cross-sectional study of overweight and obese patients. Prev Med. 2014;62:103–107. doi: 10.1016/j.ypmed.2014.02.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Wee CC, Davis RB, Huskey KW, Jones DB, Hamel MB. Quality of life among obese patients seeking weight loss surgery: the importance of obesity-related social stigma and functional status. J Gen Intern Med. 2013;28:231–238. doi: 10.1007/s11606-012-2188-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians' weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79:156–161. doi: 10.1097/00001888-200402000-00012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003;36:669–675. doi: 10.1016/s0091-7435(03)00055-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 83. Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7:35. doi: 10.1186/1471-2296-7-35. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 84. Campbell K, Engel H, Timperio A, Cooper C, Crawford D. Obesity management: Australian general practitioners' attitudes and practices. Obes Res. 2000;8:459–466. doi: 10.1038/oby.2000.57. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Hall KD, Heymsfield SB, Kemnitz JW, Klein S, Schoeller DA, Speakman JR. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012;95:989–994. doi: 10.3945/ajcn.112.036350. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 86. Burgess DJ, Warren J, Phelan S, Dovidio J, van Ryn M. Stereotype threat and health disparities: what medical educators and future physicians need to know. J Gen Intern Med. 2010;25(Suppl. 2):S169–S177. doi: 10.1007/s11606-009-1221-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Kaminsky J, Gadaleta D. A study of discrimination within the medical community as viewed by obese patients. Obes Surg. 2002;12:14–18. doi: 10.1381/096089202321144513. [ DOI ] [ PubMed ] [ Google Scholar ]
- 88. Merrill E, Grassley J. Women's stories of their experiences as overweight patients. J Adv Nurs. 2008;64:139–146. doi: 10.1111/j.1365-2648.2008.04794.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 89. Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22:882–887. doi: 10.1007/s11606-007-0160-1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. O'Reilly C, Sixsmith J. From theory to policy: reducing harms associated with the weight-centered health paradigm. Fat Stud. 2012;1:97–113. [ Google Scholar ]
- 91. Tylka TL, Annunziato RA, Burgard D, et al. The weight-inclusive versus weight-normative approach to health: evaluating the evidence for prioritizing well-being over weight loss. J Obes. 2014;2014:983495. doi: 10.1155/2014/983495. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 92. Batson CD, Lishner DA, Carpenter A, et al. ‘… As you would have them do unto you’: does imagining yourself in the other's place stimulate moral action? Pers Soc Psychol Bull. 2003;29:1190–1201. doi: 10.1177/0146167203254600. [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Puhl R, Brownell K. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 94. Danielsdottir S, O'Brien KS, Ciao A. Anti-fat prejudice reduction: a review of published studies. Obes Facts. 2010;3:47–58. doi: 10.1159/000277067. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Puhl RM, Schwartz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: a new approach for reducing bias. Health Psychol. 2005;24:517–525. doi: 10.1037/0278-6133.24.5.517. [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. Burgess DJ. Are providers more likely to contribute to healthcare disparities under high levels of cognitive load? How features of the healthcare setting may lead to biases in medical decision making. Med Decis Making. 2010;30:246–257. doi: 10.1177/0272989X09341751. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Lillis J, Hayes SC. Applying acceptance, mindfulness, and values to the reduction of prejudice: a pilot study. Behav Modif. 2007;31:389–411. doi: 10.1177/0145445506298413. [ DOI ] [ PubMed ] [ Google Scholar ]
- 98. Kemeny ME, Foltz C, Cavanagh JF, et al. Contemplative/emotion training reduces negative emotional behavior and promotes prosocial responses. Emotion. 2012;12:338–350. doi: 10.1037/a0026118. [ DOI ] [ PubMed ] [ Google Scholar ]
- 99. Faith MS, Kral TV. Social, environmental, and genetic influences on obesity and obesity-promoting behaviors: fostering research integration. In: Hernandez LM, Blazer DG, editors. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington, DC: National Academies Press; 2006. pp. 236–280. [ Google Scholar ]
- 100. Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597–1604. doi: 10.1056/NEJMoa1105816. [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. O'Brien KS, Puhl RM, Latner JD, Mir AS, Hunter JA. Reducing anti-fat prejudice in preservice health students: a randomized trial. Obesity (Silver Spring) 2010;18:2138–2144. doi: 10.1038/oby.2010.79. [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Lewis S, Thomas SL, Hyde J, Castle D, Blood RW, Komesaroff PA. ‘I don't eat a hamburger and large chips every day!’ A qualitative study of the impact of public health messages about obesity on obese adults. BMC Public Health. 2010;10:309. doi: 10.1186/1471-2458-10-309. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 103. Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [ DOI ] [ PubMed ] [ Google Scholar ]
- 104. Riddell LJ, Inman V. Body weight and weight loss: are health messages reaching their target? Asia Pac J Clin Nutr. 2007;16:683–687. [ PubMed ] [ Google Scholar ]
- 105. Yancey AK, Simon PA, McCarthy WJ, Lightstone AS, Fielding JE. Ethnic and sex variations in overweight self-perception: relationship to sedentariness. Obesity (Silver Spring) 2006;14:980–988. doi: 10.1038/oby.2006.112. [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. West DS, DiLillo V, Bursac Z, Gore SA, Greene PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care. 2007;30:1081–1087. doi: 10.2337/dc06-1966. [ DOI ] [ PubMed ] [ Google Scholar ]
- 107. Carels RA, Darby L, Cacciapaglia HM, et al. Using motivational interviewing as a supplement to obesity treatment: a stepped-care approach. Health Psychol. 2007;26:369–374. doi: 10.1037/0278-6133.26.3.369. [ DOI ] [ PubMed ] [ Google Scholar ]
- 108. Pollak KI, Alexander SC, Coffman CJ, et al. Physician communication techniques and weight loss in adults: project CHAT. Am J Prev Med. 2010;39:321–328. doi: 10.1016/j.amepre.2010.06.005. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 109. Purdie-Vaughns V, Steele CM, Davies PG, Ditlmann R, Crosby JR. Social identity contingencies: how diversity cues signal threat or safety for African Americans in mainstream institutions. J Pers Soc Psychol. 2008;94:615–630. doi: 10.1037/0022-3514.94.4.615. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (122.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
COMMENTS
Research studies on obesity and healthcare have found that most nurses believe that obesity could be prevented by self-control. Some studies find that both men and women who are taller than average are advantaged in employment situations.
Preferences for thinner people have been found among adolescents, children, parents, and even those themselves who are fat. Overweight children view social discrimination as the most immediate consequence of their weight. In some cultures, overweight is desirable. In one study, time spent watching television was associated with obesity.
Study with Quizlet and memorize flashcards containing terms like People are most likely to negatively view ______ as being a condition that could be controlled but is not due to lack of self-discipline., The prevalence of overweight has increased primarily due to, Similar to most other non-dominant group members, overweight people and more.
An analysis from the Women's Health Study found a significant association between obesity, the development of hypertension, and diabetes. 26 In this analysis of 38172 women who were free of diabetes and CVD at baseline with a mean 10.2 years of follow-up, the age-adjusted incidence rate/1000 of diabetes in obese women (BMI ≥ 30 kg/m 2) was 7. ...
Obesity, a complex medical condition, has reached epidemic proportions in the United States (US). The National Health and Nutrition Examination Survey (NHANES) conducts height and weight assessments on a representative sample of Americans to gauge its prevalence. A study by Hales et al reported that between 2013 and 2016, the prevalence of obesity stood at 36.5% for men and 40.8% for women.[1 ...
Recent research has established the physiology of weight regulation, the pathophysiology that leads to unwanted weight gain with establishment of a higher body-weight set point, and the defense of the overweight and obese state even when reasonable attempts in lifestyle improvement are made. This knowledge has informed our approach to obesity as a chronic disease. The assessment of adiposity ...
Research studies on obesity and healthcare have found that _________.Most nurses understand that obesity can be easily prevented by self-control.Overweight people are less likely to receive preventive care than others.Medical professionals do not hold the same negative perceptions that employers hold about those who are overweight.The attitude ...
Abstract. Obesity is a complex multifactorial disease that accumulated excess body fat leads to negative effects on health. Obesity continues to accelerate resulting in an unprecedented epidemic that shows no significant signs of slowing down any time soon. Raised body mass index (BMI) is a risk factor for noncommunicable diseases such as ...
Background In an era when obesity prevalence is high throughout much of the world, there is a correspondingly pervasive and strong culture of weight stigma. For example, representative studies show that some forms of weight discrimination are more prevalent even than discrimination based on race or ethnicity. Discussion In this Opinion article, we review compelling evidence that weight stigma ...
We reviewed all original studies in the fall of 2014 on topics related to obesity stigma in medical care and/or the impact of stigma on interpersonal encounters and decision-making in PubMed and PsychInfo, with the majority of studies found in health communication, social psychology and health disparities research.